
Title: ICD-10-CM Coding of Respiratory Conditions
Channel: Jennifer Lame
ICD-10-CM Coding of Respiratory Conditions by Jennifer Lame
respiratory depression icd 10 cm, respiratory distress icd 10 cm, respiratory distress syndrome icd 10 cm, acute hypoxic respiratory distress icd 10 cm, respiratory distress syndrome icd 10 code, respiratory distress unspecified icd 10 code, respiratory distress newborn icd 10 code, severe respiratory distress icd 10 code, respiratory depression icd 10
Respiratory Depression ICD-10-CM: The SHOCKING Code You NEED to Know!
Unmasking Respiratory Depression: Decoding the Silent Threat
Respiratory depression. The phrase itself whispers a chilling narrative. It's a medical enigma, often insidious, and can be profoundly dangerous. We're going to delve into this complex subject. This exploration will unveil critical information. We will be examining the ICD-10-CM code and its significance. Therefore, buckle up; we're taking a detailed look.
The Invisible Danger: Understanding Respiratory Depression
What exactly is respiratory depression? Essentially, it is a decrease in the rate and/or depth of breathing. This critical reduction compromises the body's oxygen supply. It simultaneously causes a dangerous buildup of carbon dioxide. The result can be truly frightening. Sadly, it often goes unnoticed initially. This silent nature makes early detection paramount. Imagine it as a slow but persistent encroachment on the very essence of life. Without intervention, the consequences escalate rapidly. The brain and other vital organs suffer from this deficiency.
Decoding the Code: Unveiling the ICD-10-CM Connection
Now, let’s turn our focus toward the crucial code. ICD-10-CM provides a standardized classification system. It's an international coding system for diseases and medical conditions. Respiratory depression has its designated code within this system. Knowing this specific code is fundamental. It allows for accurate diagnosis. Furthermore, it assists with effective billing and data tracking. Understanding the correct code is vital for healthcare professionals.
The Ripple Effect: Exploring the Causes and Contributing Factors
So, what sets off this cascade of respiratory distress? The triggers can be diverse. Opioid medications, in particular, are a well-known culprit. They can profoundly suppress the respiratory drive. These powerful painkillers are frequently prescribed. However, awareness of the risks is essential. Neurological disorders also play a significant role. Brain injuries, strokes, and other conditions that affect the brainstem can cause this. Furthermore, certain underlying medical conditions, such as chronic obstructive pulmonary disease (COPD), are also factors. Finally, substance abuse, including alcohol, can compound the problem. It’s a complex interplay of physiological vulnerabilities.
Symptoms That Demand Attention: Recognizing the Warning Signs
Recognizing the warning signs is truly crucial. It’s about becoming a vigilant observer. Look for subtle clues. Slow, shallow breathing is an obvious red flag. Bluish discoloration of the skin (cyanosis) indicates a lack of oxygen. Confusion, drowsiness, and disorientation are other indicators. These symptoms represent a profound physiological crisis. Early detection can make a world of difference. Patients need immediate medical attention.
The Urgent Response: Treatment Strategies and Intervention Tactics
Once respiratory depression is suspected, swift action is necessary. The immediate priority is stabilizing the patient's breathing. This often involves providing supplemental oxygen. Sometimes, more aggressive interventions are needed. Assisted ventilation might become essential. Medications, like naloxone for opioid overdoses, can be life-saving. The focus is on restoring adequate oxygenation. Therefore, healthcare professionals will work quickly. They're aiming to reverse the effects of respiratory depression.
Prevention is Paramount: Proactive Measures and Mitigation Strategies
Prevention is always better than cure. This extends to respiratory depression. Proper medication management is crucial. Careful monitoring of patients on opioids, or other respiratory depressants, is essential. Education plays a pivotal role. Healthcare providers, and patients, must understand the risks. Recognizing potential complications is always vital. Therefore, it is important to discuss the patient's condition with healthcare providers. Implementing protocols and establishing monitoring systems also helps a lot. Remember, vigilance is the most powerful tool in the fight.
The Takeaway: A Call to Action for Enhanced Awareness
Ultimately, the goal is to protect patients. Respiratory depression represents a serious threat. Understanding the condition is the first line of defense. Educating yourself, recognizing the warning signs, and knowing the importance of prompt intervention can save lives. So, be informed. Be vigilant. Be proactive. Advocate for yourself. Be prepared to act swiftly. This knowledge can make a profound impact. It might even save someone's life.
Postpartum Depression: My Reddit Disability Claim Journey (Shocking Truth!)Respiratory Depression ICD-10-CM: The SHOCKING Code You NEED to Know!
Hey everyone, let's talk about something serious, something that can sneak up on you like a shadow in the night: Respiratory Depression. I know, it sounds scary, and frankly, it is. But don't worry, we're going to break it down, making it understandable and, hopefully, a little less intimidating. Forget those dry medical textbooks – we're going to chat about it like we're at a coffee shop, okay? And trust me, knowing about this can literally save lives.
1. The Invisible Enemy: What is Respiratory Depression Anyway?
Think of your body as a finely tuned engine. Oxygen is the fuel, and your lungs are the air filters. Respiratory depression is like… well, it's like the engine getting choked, or the air filter getting blocked. Essentially, it means your breathing slows down, becomes shallow, or even stops altogether. Your body isn't getting enough oxygen, and that, my friends, is a very, very bad thing. It’s like trying to run a marathon on a single breath.
2. The Sneaky Culprit: Causes of Respiratory Depression
Now, this isn’t just one thing. It's multi-faceted. There are a ton of reasons why your breathing might decide to take a nap.
- Medications: Opioids and sedatives are the big ones. Think about it: they're designed to slow things down, and sometimes, they can overdo it.
- Underlying Health Conditions: Think about things like lung diseases (COPD, asthma), neurological problems (stroke, brain injury), and metabolic issues. They can all play a role.
- Substance Abuse: Drugs like heroin and fentanyl are infamous for causing respiratory depression.
- Physical Trauma: Chest injuries, especially those that impact the lungs, can be a significant trigger.
3. ICD-10-CM: The Code That Matters
Here’s where we get to the nitty-gritty. The coding system used by doctors and hospitals to categorize diagnoses is the "ICD-10-CM." For respiratory depression, there's a specific code (or codes!), and it's incredibly important. Why? Because it helps track the prevalence of the condition, informs treatment, and is vital for billing and research. It allows health professionals to communicate effectively and consistently. We’re not going to dive into the exact codes because, frankly, that's for the pros. But understanding that these codes exist and are crucial is the key takeaway here.
4. Recognizing the Danger Signs: Symptoms You Can't Ignore
This is where paying attention becomes absolutely vital. Time is of the essence. If you or someone you know shows any of these signs, get help immediately:
- Slow, shallow breathing: Think of it like a tortoise race, instead of a cheetah sprint.
- Bluish discoloration of the skin, lips, or fingernails (cyanosis): This is a tell-tale sign of oxygen deprivation. It’s like your body is slowly turning blue.
- Drowsiness or confusion: Like it’s hard to focus. Imagine trying to solve a complex puzzle while you’re extremely tired.
- Loss of consciousness: This is the most frightening sign.
- Gasping for air.
5. The Importance of Early Detection: Why Time is Of The Essence
Imagine a ticking time bomb. Every second counts. Respiratory depression can progress from a slight slowing of breathing to a complete cessation of breath in a matter of minutes. Early detection is the key to saving a life. Think of it as catching the first crack in a dam. The sooner you act, the better the chances of preventing a catastrophe.
6. Treatment Strategies: What Can Be Done?
The specifics of treatment depend on the cause and severity, but it's all about getting oxygen into the body and addressing the underlying problem.
- Supplemental Oxygen: This is often the first step.
- Medications: Sometimes, medications can reverse the effects of drugs that caused the depression.
- Mechanical Ventilation: In severe cases, a ventilator provides breathing support.
- Addressing the Underlying Cause.
7. The Role Of Naloxone: A Lifesaver in Opioid Overdoses
Naloxone (Narcan) is a miracle drug, especially when it comes to opioid overdoses. It can rapidly reverse the effects of opioids, including respiratory depression. If you suspect an opioid overdose, call for help immediately and administer naloxone if it's available. It is an essential line of defense.
8. Risk Factors: Who Is Most Vulnerable?
Certain people are at higher risk. Being aware of these risk factors is critical for prevention:
- People taking opioid medications, especially in combination with other sedatives.
- Individuals with existing respiratory conditions.
- Those with a history of substance abuse.
- Older adults.
- Those with sleep apnea.
9. Prevention is Paramount: Ways To Safeguard Yourself and Others
This is all about being proactive. Always take medication exactly as prescribed. Know the signs of respiratory depression and the risks involved.
- Educate yourself and your loved ones: Understanding the risks is the first line of defense.
- Be aware of medication interactions: Talk to your doctor or pharmacist about the potential side effects of your medications.
- Carry naloxone if you or someone you know is at risk of an opioid overdose.
10. Respiratory Depression and Sleep Apnea: A Dangerous Duo
If you have sleep apnea and you're taking medications that depress breathing, you're walking a tightrope. Sleep apnea already causes periods of stopped breathing during sleep, and adding the effects of medications can be a recipe for disaster. It's critical to manage both conditions.
11. The Opioid Crisis and Respiratory Depression: A Deadly Connection
The opioid crisis has fueled a massive increase in respiratory depression cases. It's a public health emergency. We all need to be aware of the dangers.
12. Seeking Professional Help: When To Call the Doctor
Don't hesitate to seek medical attention if you or someone you know exhibits any symptoms of respiratory depression. Call emergency services immediately. Don’t wait. Time is of the essence.
13. The Emotional Toll: Coping With Respiratory Depression
This can be incredibly frightening for both the person experiencing it and for their loved ones. Support systems, including counseling and support groups, can be invaluable. Don't be afraid to reach out.
14. The Role of Healthcare Professionals: A Critical Alliance
Doctors, nurses, paramedics – they are all on the front lines. They have the tools and expertise to diagnose and treat respiratory depression. Trust their judgment. Remember, every life matters.
15. The Future of Respiratory Depression: Ongoing Research and Innovations
We're not sitting still. Research continues to advance our understanding, leading to better treatments and prevention strategies. Think about cutting-edge technology and more nuanced approaches. There's always hope.
Closing Thoughts
Respiratory depression is a serious issue, but it's not a sentence. By understanding the risks, recognizing the symptoms, and knowing how to react, we can all play a role in saving lives. It's all about being informed, being prepared, and being ready to act when it matters most. Stay safe out there, and remember, you are not alone.
FAQs
What is the main cause of respiratory depression? Respiratory depression has multiple causes, but the most common are medications (especially opioids and sedatives), underlying health conditions (like lung disease), substance abuse, and trauma.
How is respiratory depression diagnosed? Diagnosis involves a physical examination, checking vital signs (breathing rate, oxygen saturation), and sometimes blood tests to measure oxygen and carbon dioxide levels.
Can respiratory depression be prevented? Yes. Prevention involves things like taking medications only as prescribed, avoiding combining medications that depress breathing, being aware of risk factors, and carrying naloxone if appropriate.
What should I do if someone shows signs of respiratory depression? Call emergency services immediately. Check if the person is responsive. If they are not breathing or are only gasping, give rescue breaths. If naloxone is available and you suspect an opioid overdose, administer it.
Where can I find more information about respiratory depression? Talk to your doctor, visit reputable medical websites (like the CDC or NIH), or look for support groups and educational resources.
1) Principal Keywords: Respiratory Depression, ICD-10-CM 2) SEO Headline: Respiratory Depression: The SHOCKING Code You Need! 3) Pathway: Respiratory Depression 4) Meta Summary: Uncover the SHOCKING truth about Respiratory Depression and the critical ICD-10-CM code. Learn vital signs, treatment, and prevention. Stay informed! 5) Image Alt Text: Person in oxygen mask, with text "Respiratory Depression Information"
Depression Cherry: The SHOCKING Reason It's Album of the Year!ICD 10 CM Coding COPD coding explained

By Medical Coding Clarified ICD 10 CM Coding COPD coding explained by Medical Coding Clarified
ICD-10-CM Chapter 10 Diseases of the Respiratory System J00J99 Medical Coding

By Professional Certifications ICD-10-CM Chapter 10 Diseases of the Respiratory System J00J99 Medical Coding by Professional Certifications
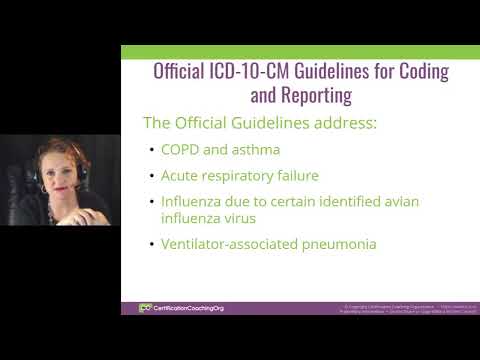
Title: ICD-10-CM - Diseases of the Respiratory System
Channel: MedicalCodingCert
ICD-10-CM - Diseases of the Respiratory System by MedicalCodingCert
Pregnant & Depressed? Reddit's Shocking Secret Confessions Will Leave You Speechless
Respiratory Depression ICD-10-CM: Unveiling the Critical Codes
The shadows of medical complexity often obscure vital details. When it comes to respiratory health, the stakes are undeniably high. Understanding the subtle nuances of respiratory depression, and the corresponding codes within the ICD-10-CM system, is paramount for accurate diagnosis, effective treatment, and ultimately, patient well-being. This article delves into the crucial codes and their implications, providing a comprehensive and insightful guide for medical professionals.
Deciphering Respiratory Depression: Defining the Danger
Respiratory depression represents a critical medical condition characterized by a reduction in the rate and/or depth of breathing, leading to inadequate ventilation. This physiological impairment can result in a life-threatening buildup of carbon dioxide (hypercapnia) and a decrease in oxygen levels in the blood (hypoxemia). The underlying causes are numerous and diverse, ranging from medication effects to underlying medical conditions. Recognizing the signs and symptoms, along with accurate coding, is a fundamental aspect of clinical practice.
The ICD-10-CM Code Landscape: Navigating the Alphabetical Index
The ICD-10-CM system provides a standardized framework for classifying and reporting medical diagnoses. For respiratory depression, several codes are particularly relevant. Begin your search within the index by referencing "Depression, respiratory." This initial step quickly directs us towards the crucial category, offering a starting point for precise code selection. The index provides a list that reflects several different conditions. Ensure a precise match to the clinical presentation to avoid errors.
Exploring the Core Codes: A Detailed Examination
Several specific codes warrant close examination when coding for respiratory depression. Let's examine them, uncovering their unique applications along with specific requirements for their use.
R06.0 – Dyspnea: Although Dyspnea (Shortness of Breath) is not respiratory depression itself, it is a symptom that can be present with respiratory depression. It is important to code both conditions when they are present. This code acts as a signal of respiratory distress, requiring further investigation.
R06.2 – Wheezing: Wheezing is a high-pitched whistling sound produced by narrowed airways. While not the primary diagnosis of respiratory depression, wheezing may accompany the condition, especially in patients with underlying respiratory issues like asthma or COPD.
R06.81 – Apnea, Not Elsewhere Classified: Apnea signifies a cessation of breathing. It's a serious symptom of respiratory depression, particularly when prolonged. This requires immediate interventions. This code is a crucial consideration. Its use requires careful assessment to determine the cause of apnea and to ensure accuracy in coding.
R06.89 – Other Abnormalities of Breathing: This broad category encompasses various breathing abnormalities, including shallow breathing and irregular patterns, which can be associated with respiratory depression. This section becomes a catch-all for manifestations of respiratory depression that may not fit neatly into other, more specific categories.
J96.0 – Acute Respiratory Failure: Respiratory failure represents a critical state where the respiratory system fails to adequately oxygenate the blood and/or remove carbon dioxide, causing a patient's respiratory effort is impaired. When respiratory depression is the cause, J96.0 is the code.
J96.9 – Respiratory Failure, Unspecified: This code is for cases where the specific cause of respiratory failure is not known.
G24.0 – Drug-Induced Dystonia: This particular code holds significance, especially in cases of drug-induced respiratory depression (often caused by opioids, benzodiazepines, or other central nervous system depressants). Code this condition if the respiratory depression is directly linked to medication.
T40.0x – Poisoning by Opioids (Narcotics): This code is essential when respiratory depression is due to opioid overdose.
The Importance of Specificity: Avoiding Coding Pitfalls
Precision is non-negotiable when assigning ICD-10-CM codes. Using the most specific code possible is vital. For instance, if respiratory depression results from medication, the code should reflect the specific drug involved, when possible. Avoid using nonspecific codes when a more detailed option exists. Consult the medical record meticulously to accurately capture the complete clinical picture. Failure to capture the specific causes can introduce ambiguity, potential inaccuracies in data analysis, and could impede appropriate care.
Linking Diagnosis and Documentation: The Path to Accurate Coding
The foundation of accurate medical coding is clear, concise, and comprehensive documentation. Ensure that the medical record fully reflects the patient's presentation, the diagnostic process, and the therapeutic interventions. Document the rate and depth of respirations, oxygen saturation levels, arterial blood gas findings, and any medications administered. All relevant information must be linked and related.
Without detailed documentation, accurate coding will be impossible. The medical record should also include the physical exam findings, the patient's medical history, and the results of any diagnostic tests. All information should be presented in an organized and systematic format.
Clinical Scenarios and Coding Examples: Applying Knowledge to Practice
Here are some clinical scenarios to illustrate the application of these codes:
Scenario 1: A patient presents with shallow, slow breathing (respiratory rate of 8 breaths/minute) after receiving an opioid analgesic for post-operative pain. Oxygen saturation is 88%.
- Coding: R06.89 (Other abnormalities of breathing) or J96.0 (Acute respiratory failure) or J96.9 (Respiratory failure, unspecified) depending on clinical severity.
Scenario 2: A patient with a history of asthma develops respiratory depression due to an exacerbation of their asthma. The patient's breathing becomes labored, and they exhibit wheezing.
- Coding: J45.90 (Asthma, unspecified, uncomplicated) and R06.2 (Wheezing). In severe cases, it can be coded with respiratory failure.
Scenario 3: A patient is found unresponsive with no breathing after an accidental ingestion of a large dose of heroin.
- Coding: T40.1x (Poisoning by heroin), R06.0 (Dyspnea), R06.81 (Apnea, not elsewhere classified), and J96.0 (Acute respiratory failure) depending on the severity of the condition.
Enhancing Accuracy: Essential Code Guidelines
- Always consult the ICD-10-CM codebook and any relevant coding guidelines, particularly those issued by the Centers for Medicare & Medicaid Services (CMS).
- Familiarize yourself with coding conventions, such as the "code also" and "use additional code" guidelines. These directives are crucial for accurate and comprehensive coding.
- Utilize the codebook's index and tabular list to verify and validate the appropriate code. Never assume a code's meaning.
- Consider coding resources and training programs to increase your coding efficiency and refine your accuracy.
- If any doubt exists, consult with a certified professional.
The Impact of Accurate Coding: Beyond the Numbers
Accurate ICD-10-CM coding for respiratory depression does more than just fulfill administrative requirements. It is crucial in several critical areas:
- Patient Safety: Accurate coding helps in providing the right information for the patients. It helps in the early alerts and identifying the patient's risk factors.
- Quality Improvement: The data collected through precise coding enables healthcare organizations to assess and improve the quality of care. This includes monitoring trends, evaluating the effectiveness of treatments, and identifying areas for further research.
- Resource Allocation: Understand the frequency, severity, and causes of respiratory depression to aid in the allocation of resources, such as staffing, equipment, and educational programs.
- Public Health: Accurate coding contributes to the larger public health picture by providing data for epidemiological studies and public health interventions.
Conclusion: Mastering the Codes for Enhanced Patient Outcomes
Understanding the coding requirements for respiratory depression is critical. By mastering the core codes, embracing specificity, and adhering to the fundamental principles of clear documentation, medical professionals can contribute to better patient outcomes. The journey through the complexities of ICD-10-CM is an ongoing one. Continued education, adherence to best practices, and an unwavering commitment to accuracy will ensure the best care for those affected by respiratory depression.

