
Title: Depression CAUSES, SYMPTOMS, ICD-10 CRITERIA & MANAGEMENT
Channel: Medicine Made Simple
Depression CAUSES, SYMPTOMS, ICD-10 CRITERIA & MANAGEMENT by Medicine Made Simple
depression with sleep disturbance icd 10, depression with insomnia icd 10, other sleep disturbance icd 10, icd 10 code for insomnia due to depression, sleep pattern disturbance icd 10, sleep disturbances icd 10
Insomnia & Depression: The Shocking ICD-10 Code You NEED to Know
Unraveling the Sleep-Deprived Mind: Depression's Hidden Link
Ever feel like your mind is a tangled web, sleep a distant memory? You are not alone. Because for many, the shadows of sleepless nights and the bleakness of depression dance a disturbing tango. It's a connection often overlooked, but one with significant implications. Let's explore this complex relationship. We will journey through the intricacies of sleep and mental health.
The Silent Thief: How Insomnia Fuels the Darkness
Imagine the insidious grip of sleeplessness slowly smothering your joy. Insomnia isn't just about tossing and turning. It's a relentless thief. It steals your energy, your focus, and your emotional resilience. Consequently, it often sets the stage for something more sinister. But how does this happen?
Firstly, chronic sleep deprivation alters brain chemistry. It impairs the delicate balance of neurotransmitters. Serotonin and dopamine, vital for mood regulation, become disrupted. Moreover, this imbalance can trigger or worsen depressive symptoms. Hence, those restless nights may be the initial prelude to a deeper struggle.
Deciphering the Mental Distress: The ICD-10 Code Revealed
You're probably wondering about the specifics. The ICD-10 code that whispers this unsettling tale? It's a code doctors use. It categorizes diseases and health conditions. The code can unlock a deeper understanding of the interconnectedness. It's the code that helps health professionals diagnose and categorize these intertwined conditions.
Navigating the Maze: Finding Hope and Healing
Now, finding solutions is paramount. If this resonates with you, take heart. Healing is possible. There are strategies to navigate this maze. There are steps you can take to regain control of your sleep and your mental health. Firstly, it is very important to seek professional help. A doctor or therapist can assess your needs. They can offer tailored treatment options. This might involve medication, therapy, or a combination. Therefore, please schedule an appointment.
Secondly, consider establishing healthy sleep habits. Create a relaxing bedtime routine. Make your bedroom a sleep sanctuary. Avoid screens before bed. So, these changes will benefit your body and mind.
Thirdly, practice mindfulness and stress reduction techniques. Yoga, meditation, and deep breathing can calm your nervous system. Therefore, these practices can promote relaxation and better sleep.
The Intertwined Path: Making Informed Choices
This connection changes the way you view your well-being. It highlights the necessity of a holistic approach. Mental and physical health are intricately linked. They significantly impact each other. Your decisions will influence your health outcomes.
Ultimately, understanding this relationship is essential. It unlocks the potential for healing. It helps us make informed choices about our health. Early intervention and a proactive approach can improve your quality of life.
Empowering Yourself: Taking Control of Your Sleep and Mood
It’s time to reclaim your life from the clutches of insomnia and depression. Start by taking action. Take control of your situation. Become proactive in your health. You can empower yourself.
Therefore, educate yourself. Gather resources. Because knowledge is power. Speak with healthcare professionals. In addition, create a support system, and make the right choices.
Finally, remember that the journey to wellness is yours. You have the power to make positive changes. Embrace the strategies discussed. Because a brighter, more restful future awaits!
Depression Awareness Week 2023: Shocking Stats You NEED To See!Insomnia & Depression: The Shocking ICD-10 Code You NEED to Know
Hey there, fellow travelers on the winding road of life! We all know the feeling, right? That heavy cloud of exhaustion that just won't lift, the persistent weight on your chest, and the gnawing feeling that something just isn't quite right. Today, we're diving deep into a particularly tricky pair: insomnia and depression. We'll be unraveling their intertwined dance and, most importantly, unveiling the hidden key – the ICD-10 code – that can unlock understanding and, ultimately, pave the way to healing. Trust me, this isn't going to be some dry, medical textbook regurgitation. We're going to get personal, relatable, and utterly real. Ready? Let's get started!
1. The Unholy Alliance: Insomnia & Depression – A Love Story (Gone Wrong)
Think of insomnia and depression as two sides of a twisted coin. They often go hand in hand, a frustrating partnership that can feel impossible to break. One fuels the other, creating a vicious cycle that leaves you feeling utterly drained and hopeless. It’s like a seesaw; when one side dips, the other inevitably follows. Insomnia, the inability to fall asleep or stay asleep, leaves you physically and mentally exhausted, making it harder to cope with the challenges of daily life. This can quickly lead to feelings of sadness, hopelessness, and a loss of interest in activities you once enjoyed – prime territory for depression to flourish.
2. What's the Big Deal? Understanding the Core Issues
Okay, let's get down to brass tacks. Why are insomnia and depression such a big deal? Well, beyond the obvious – feeling lousy all the time – these conditions can significantly impact your overall well-being. They can affect your relationships, your work performance, and even your physical health. Think of it like this: your brain is like a computer. Without proper "sleep mode" (insomnia), the system malfunctions. And when the system malfunctions, it throws off the entire operation (depression). Ignoring these issues isn't an option; it's like trying to drive a car with a flat tire. Eventually, something’s gotta give.
3. The Sneaky Symptoms: Spotting the Signs Early On
Sometimes, it's tough to know when you're actually experiencing insomnia and depression, especially when their symptoms overlap. Are you just having a bad week, or is something more serious brewing? Here's a quick rundown of some telltale signs:
- Insomnia: Difficulty falling asleep, struggling to stay asleep (waking up frequently), feeling unrested even after sleep, daytime sleepiness, irritability, difficulty concentrating.
- Depression: Persistent sadness, loss of interest in activities, changes in appetite or weight, feelings of worthlessness, fatigue, difficulty concentrating, thoughts of death or suicide.
If you're experiencing several of these symptoms consistently, it's crucial to seek help. Remember, it's okay to not be okay, and there's absolutely no shame in reaching out.
4. Enter the ICD-10 Code: The Secret Weapon
Now, for the grand reveal! The ICD-10 code – the International Classification of Diseases, Tenth Revision – is a diagnostic tool used by healthcare professionals to classify and code all known diseases and health problems. When it comes to insomnia and depression, the codes help doctors accurately diagnose and treat these conditions. The key, the one we're after, is that understanding these codes allows a more precise diagnosis and can therefore lead to better treatment.
5. Deciphering the Codes: A Simplified Guide
Let's keep it simple. Instead of overwhelming you with a laundry list of codes, let's focus on the general categories. Remember, I'm not a doctor; this is just for informational purposes! Your doctor will determine the exact codes for your specific situation.
- F51.0: Insomnia (nonorganic) – This code is often used when insomnia isn't caused by a specific medical condition or substance use.
- F32: Depressive episode – This is the general category for a depressive episode, ranging in severity.
- F33: Recurrent depressive disorder – This code applies to those who have experienced multiple episodes of depression.
- Important Note: There are numerous subcategories within these broader classifications, and a doctor will determine the specific code based on your symptoms and medical history.
The point is, the ICD-10 code is a tool, a language that healthcare professionals use to understand and treat your specific condition.
6. Why the Code Matters: More than Just Numbers
You might be thinking, "So what? It's just a code." But it's so much more than that. The ICD-10 code provides a common language for healthcare providers, ensuring accurate communication and facilitating appropriate treatment. It also plays a crucial role in billing and insurance purposes. Think of it as the key that unlocks the door to getting the help you need.
7. The Chicken or the Egg? Figuring Out the Cause
Which came first, the insomnia or the depression? This is the classic chicken-or-the-egg scenario, and truthfully, the answer varies from person to person. Sometimes, sleep problems trigger depression. Other times, depression comes first, wreaking havoc on your sleep patterns. Often, the two are intertwined. The good news is that by tackling both insomnia and depression simultaneously, you stand a much better chance of finding relief.
8. Treatment Strategies: A Multifaceted Approach
There's no one-size-fits-all solution, and that's okay. Treatment for insomnia and depression typically involves a combination of approaches, customized to your specific needs. This can include:
- Therapy: Cognitive Behavioral Therapy for Insomnia (CBT-I) – a highly effective non-medication approach for sleep issues, and talk therapy, such as Cognitive Behavioral Therapy (CBT) or interpersonal therapy to address the root causes of depression.
- Medication: Antidepressants and/or sleep aids, prescribed by a doctor.
- Lifestyle Changes: Regular exercise (but not too close to bedtime!), a healthy diet, avoiding caffeine and alcohol before bed, and establishing a consistent sleep schedule.
- Mindfulness and Relaxation Techniques: Meditation, deep breathing exercises, and other practices that help you relax and manage stress.
9. The CBT-I Advantage: Taking Control of Your Sleep
As mentioned, Cognitive Behavioral Therapy for Insomnia (CBT-I) is a game-changer. It's a structured program that teaches you how to change the thoughts and behaviors that are contributing to your sleep problems. Think of it as re-training your brain to sleep. It's incredibly empowering and can be more effective than medication in the long run.
10. Medication Matters: Navigating the Options
While medication isn't always the answer, it can be a lifesaver for some. Antidepressants can help regulate mood, and sleep aids can provide temporary relief from insomnia. However, it's crucial to work closely with your doctor to weigh the benefits and risks, discuss potential side effects, and monitor your progress. Remember, medication is often most effective when combined with therapy and lifestyle changes.
11. Lifestyle Hacks: Putting the Odds in Your Favor
Beyond therapy and medication, you have immense power to improve your sleep and mood through simple lifestyle adjustments. Here are a few ideas:
- Create a consistent sleep schedule: Go to bed and wake up at the same time every day, even on weekends.
- Optimize your sleep environment: Make sure your bedroom is dark, quiet, and cool.
- Limit screen time before bed: The blue light emitted by electronic devices can interfere with sleep.
- Practice relaxation techniques: Deep breathing, meditation, and progressive muscle relaxation can help you wind down before bed.
- Exercise regularly: But avoid strenuous workouts close to bedtime.
- Watch your diet: Avoid sugary drinks and excessive caffeine, especially in the afternoon and evening.
- Consider a gratitude journal: Focusing on the positive aspects of your life can help combat feelings of depression.
12. The Importance of Self-Care: Your Mental Health Toolkit
Taking care of yourself is non-negotiable, especially when you're dealing with insomnia and depression. Think of self-care as your mental health toolkit. It's about doing things that nourish your mind, body, and soul. This might include:
- Spending time in nature: A walk in the park or a hike in the woods can do wonders for your mood.
- Connecting with loved ones: Social support is crucial.
- Engaging in activities you enjoy: Reading, listening to music, painting – whatever brings you joy.
- Practicing mindfulness: Paying attention to the present moment without judgment.
- Setting boundaries: Saying "no" to things that drain your energy.
13. When to Seek Professional Help: Don't Go It Alone
While self-care and lifestyle changes can be incredibly helpful, it's essential to recognize when you need professional help. If you're experiencing persistent symptoms of insomnia and/or depression, if your symptoms are interfering with your daily life, or if you're having thoughts of harming yourself or others, please reach out to a mental health professional or your doctor. Don't suffer in silence. Help is available, and you don't have to go through this alone.
Escape the Darkness: Proven Coping Mechanisms for Depression
Using ICD-9 and ICD-10 Codes to Bill for Depression Care

By National Council for Mental Wellbeing Using ICD-9 and ICD-10 Codes to Bill for Depression Care by National Council for Mental Wellbeing
ICD 10 Documentation Education Mental and Behavioral Disorders
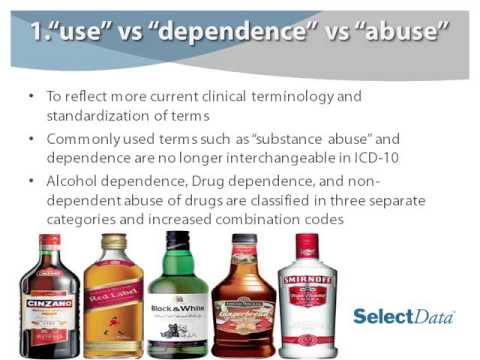
By CHS at Select Data ICD 10 Documentation Education Mental and Behavioral Disorders by CHS at Select Data
ICD 10 diagnostic criteria for Insomnia

By Vijay Bhatia ICD 10 diagnostic criteria for Insomnia by Vijay Bhatia

Title: ICD 10 diagnostic criteria for Hypersomnia Excessive sleep disorder
Channel: Vijay Bhatia
ICD 10 diagnostic criteria for Hypersomnia Excessive sleep disorder by Vijay Bhatia
Depression & Eating Disorders: The Shocking Connection You NEED To Know
Insomnia & Depression: The Shocking ICD-10 Code You NEED to Know
Navigating the labyrinthine world of mental health can feel overwhelming. From pinpointing the root causes of our struggles to deciphering the complex language of medical professionals, it's a journey often paved with uncertainty. Today, we are going to shed light on a crucial element in this journey: the intersection of insomnia, depression, and the specific coding system used to diagnose and treat them. We will uncover the vital ICD-10 code you absolutely need to know, empowering you with the knowledge to advocate for your well-being.
The Silent Epidemic: Understanding the Intertwined Nature of Insomnia and Depression
Before plunging into the specifics of the ICD-10 code, it's vital to recognize the profound link between insomnia and depression. These two conditions often exist in a vicious cycle, each exacerbating the other. Chronic insomnia, the persistent difficulty falling asleep, staying asleep, or experiencing restful sleep, can significantly contribute to the development of depressive symptoms. Sleepless nights can erode our emotional resilience, making us more vulnerable to feelings of sadness, hopelessness, and a loss of interest in activities we once enjoyed.
Conversely, depression frequently manifests as sleep disturbances. Many individuals grappling with depression experience insomnia, while others may find themselves sleeping excessively, a condition often referred to as hypersomnia. The interplay is complex, with both biological and psychological factors contributing to the connection. Brain chemistry, particularly the regulation of neurotransmitters like serotonin and dopamine, plays a crucial role in both sleep and mood. The stress and emotional turmoil inherent in depression can further disrupt sleep patterns, reinforcing the cycle. Addressing both insomnia and depression simultaneously is often the most effective path toward recovery.
Decoding the ICD-10: The Language of Diagnosis
The International Classification of Diseases, Tenth Revision (ICD-10) is the global standard diagnostic tool for epidemiology, health management, and clinical purposes. Developed and maintained by the World Health Organization (WHO), the ICD-10 provides a standardized system for classifying diseases and health problems. It allows healthcare providers to accurately document diagnoses, track disease trends, and communicate effectively across different healthcare settings and countries. Each condition is assigned a unique code, facilitating data collection and research.
Unveiling the Key Code: F51.0 – Nonorganic Insomnia
The specific ICD-10 code that we will focus on is F51.0 – Nonorganic insomnia. This code is used to classify sleep disturbances that are not directly caused by a physical illness, substance use, or another psychiatric disorder. "Nonorganic" indicates that the primary cause of the insomnia is related to psychological factors. This code is particularly relevant when the insomnia is linked to, or contributes to, symptoms of depression. While other codes may be applicable—such as those specifically addressing depressive episodes—F51.0 is crucial for acknowledging the sleep disruption as a significant component of the patient's overall condition.
Understanding the nuances of F51.0 is crucial. It's not just a label; it's a signal to healthcare providers to delve deeper into the underlying factors contributing to the insomnia. This may involve a thorough assessment of the patient's sleep patterns, mood, stress levels, and any potential environmental or psychological triggers. The accurate use of this code also informs the development of a tailored treatment plan.
The Importance of Accurate Diagnosis and Coding
The correct application of the ICD-10 code has far-reaching implications. For individuals, it can mean access to appropriate care and treatment. It ensures that healthcare professionals are aware of the specific challenges you are facing, allowing them to personalize your treatment plan and provide comprehensive support.
Accurate coding also has benefits that extend beyond individual care. It helps healthcare systems track the prevalence of specific conditions, allocate resources effectively, and monitor the success of different treatment approaches. Research relies heavily on accurate coding to understand disease patterns, identify risk factors, and develop new interventions. Finally, a proper diagnosis using the ICD-10 ensures that you can access any necessary medical insurance coverage or disability benefits.
Exploring the Treatment Landscape: Strategies for Managing Insomnia and Depression
Treatment for insomnia and depression typically involves a multifaceted approach. Recognizing that these conditions are often interconnected, healthcare providers will often recommend interventions targeting both.
Therapy: Cognitive Behavioral Therapy for Insomnia (CBT-I) is a highly effective, non-pharmacological treatment that helps individuals change the thoughts and behaviors that contribute to insomnia. CBT-I may include techniques such as sleep restriction, stimulus control, and cognitive restructuring, which aim to improve sleep hygiene and address negative thought patterns about sleep. Simultaneously, therapies like Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT) are frequently utilized to address the underlying depression. These therapies can help individuals identify and challenge negative thought patterns, improve communication skills, and develop coping mechanisms.
Medication: Antidepressants are often prescribed to treat depression, and some of these medications can also have beneficial effects on sleep. Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are commonly prescribed as first-line treatments for depression. For individuals with insomnia, a physician may prescribe sleep aids, such as benzodiazepines or non-benzodiazepine hypnotics. However, these medications often have side effects and can be habit-forming, so their use should be closely monitored by a healthcare professional.
Lifestyle Adjustments: Making positive changes to daily habits can significantly improve both insomnia and depression symptoms. This includes establishing a regular sleep schedule, creating a relaxing bedtime routine, avoiding caffeine and alcohol before bed, and exercising regularly. Dietary adjustments, such as minimizing processed foods and incorporating nutrient-rich foods, can play a crucial role in overall well-being.
Complementary and Alternative Approaches: Some individuals find relief from symptoms through complementary therapies, such as acupuncture, yoga, mindfulness meditation, and herbal remedies. While research on the effectiveness of these approaches is ongoing, they may be a valuable addition to a comprehensive treatment plan.
Advocating for Yourself: Steps You Can Take
Navigating the complexities of mental health care requires proactive self-advocacy. Here are some steps you can take to ensure you receive the best possible support:
- Detailed Documentation: Keep a sleep diary, recording when you go to bed, when you wake up, how you feel, and any factors that might be affecting your sleep. Also, note any symptoms of depression you are experiencing. This information is invaluable to your healthcare provider.
- Open Communication: Be honest and open with your healthcare provider about your symptoms, concerns, and any challenges you are facing. Don't hesitate to ask questions and seek clarification.
- Seek a Specialist: If you feel your primary care physician is not providing adequate support, consider consulting with a psychiatrist, psychologist, or sleep specialist.
- Research and Education: Educate yourself about insomnia and depression. The more you understand these conditions, the better equipped you will be to make informed decisions about your care.
- Second Opinions: Do not be afraid to seek a second opinion if you have any doubts about your diagnosis or treatment plan.
The Path Forward: Finding Hope and Healing
The journey through insomnia and depression can be challenging, but it is not a solitary one. By understanding the critical link between these conditions, familiarizing yourself with the relevant ICD-10 code, and actively participating in your care, you can regain control and embark on the path toward healing. Remember, seeking help is a sign of strength. With the right support, you can overcome these obstacles and rediscover the joy and fulfillment that life offers. The key to recovery lies in your active participation, informed decisions, and a dedicated partnership with healthcare providers. Take the first step today, and start building a brighter tomorrow.
