Title: The Geriatric Depression Scale GDS Assessment
Channel: HIGN at NYU Meyers
The Geriatric Depression Scale GDS Assessment by HIGN at NYU Meyers
depression screening elderly, depression screening older adults, depression screening tool for elderly, depression screening age, depression in older adults guidelines, what is depression in the elderly
Is Your Elderly Loved One Hiding Depression? Urgent Screening Needed!
Is Mom or Dad Secretly Sad? Unmasking Depression in Your Elderly Family Member
It’s a chilling thought, isn't it? The people you cherish, the ones who shaped your world, might be struggling in silence. Depression in the elderly is a silent thief. It creeps in subtly, often masked by the aging process. But don’t let it remain a secret. Recognizing the signs early makes a massive difference. Let's explore how you can help.
The Unseen Struggle: Why Depression Often Goes Undetected
Think about it: life throws curveballs. For seniors, these can be especially daunting. Loss of loved ones, chronic health issues, and social isolation all contribute. Yet, many elderly individuals downplay their feelings. They might not want to burden anyone. Or, they might believe it's just a part of getting older.
Consequently, families often miss the subtle cues. Furthermore, standard aging symptoms can mirror depression. Fatigue, changes in appetite, and sleep disturbances are all potential red flags. Therefore, it's crucial to look beyond the obvious. Instead, delve deeper into their emotional state.
Spotting the Subtle Clues: Beyond the Everyday
So, what should you be looking for? Notice changes in their usual behavior. Are they suddenly losing interest in hobbies they once loved? Do they withdraw from social activities? These seemingly small shifts can be significant.
Also, pay attention to their physical health. Depression can manifest as aches and pains with no clear physical cause. Are they complaining of persistent fatigue? Do they seem to be neglecting their personal hygiene? Changes in sleep patterns, like sleeping too much or too little, are also key indicators.
Moreover, subtle changes in mood are critical to observe. Irritability, anger, and hopelessness are common. They might express feelings of worthlessness or guilt. These aren’t just bad days; it could be something more. Remember, it is paramount to encourage open communication.
Facilitating Open Dialogue: Breaking Down Barriers
Talking can be the hardest part. Your loved one might be resistant to sharing their feelings. They may fear being a burden, or they might not understand what’s happening. Therefore, you need to approach the conversation with sensitivity and patience.
First, pick the right time and setting. Choose a quiet place where they feel comfortable and relaxed. Start by simply expressing your concern. Use "I" statements: "I've noticed you haven't been yourself lately."
Further, listen more than you talk. Allow them to express their feelings without interruption. Validate their emotions. Let them know it’s okay to feel sad, angry, or frustrated. Most importantly, resist the urge to give quick fixes.
In addition, avoid judgmental language. Instead, offer gentle encouragement. Let them know you're there to support them. If they're unwilling to talk, don’t force it. Instead, try again later. Building trust takes time.
Seeking Professional Support: A Crucial Next Step
If you suspect depression, professional help is vital. Don’t delay seeking assistance. Schedule an appointment with their primary care physician. They can conduct a thorough assessment. A doctor can also rule out other medical conditions.
Also, consider a consultation with a geriatric psychiatrist or a therapist specializing in elderly care. They are well-equipped to address specific challenges faced by seniors. Therapy, such as cognitive-behavioral therapy, has proven effective in treating depression.
Furthermore, medication might be necessary. A psychiatrist can explore the best options. The most effective treatment plans often include a combination of therapy and medication. Remember, this is an ongoing process.
Empowering Your Loved One: Strategies for Well-being
Besides professional help, there are things you can do at home. Encourage them to maintain a healthy lifestyle. Regular exercise, a balanced diet, and adequate sleep are essential. They can significantly improve mood.
Additionally, foster social connections. Isolation can worsen depression. Encourage them to stay involved in activities they enjoy. Facilitate regular visits with family and friends. Consider joining senior groups or clubs.
Moreover, create a supportive environment. Offer practical help. Assist with daily tasks if needed. Show patience and understanding. Remind them they are loved and valued. Small gestures make a big difference.
Navigating the Journey: Hope and Healing
Dealing with depression in an elderly loved one is not easy. However, recognizing the issue and seeking help is important. There is hope, and recovery is achievable. With the right support and treatment, they can regain their quality of life.
Remember, it's a marathon, not a sprint. There will be ups and downs. Therefore, be patient. Celebrate small victories along the way. Most importantly, never give up. Your love and support are invaluable. By working together, you can help them find their way back to happiness.
Is This Depression? Take Our Quick Test NOW!Is Your Elderly Loved One Hiding Depression? Urgent Screening Needed!
We've all been there, haven't we? That nagging feeling in the back of our minds, that quiet worry for a loved one. Especially when it comes to our elders. They've weathered the storms of life, seen so much, and perhaps, developed an almost Zen-like ability to mask their true feelings. But sometimes, that masking can be a symptom in itself. And the biggest worry of all is depression. It's a silent thief, chipping away at their joy, their energy, their very will to live. So, how do we know if our elderly loved one is really okay? How do we discern if they're just "getting older" or genuinely struggling with depression? Let's dive in.
1. The Shadow of Silence: Understanding Depression in Seniors
Depression in the elderly is often overlooked, even by the people who love them the most. Why? Because the symptoms, the tell-tale signs, can easily be dismissed as typical signs of aging. Forgetfulness? "Oh, that's just Dad getting older." Loss of appetite? "He's always been a picky eater." Withdrawal from social activities? "He's tired, he just wants to rest." But what if these are more than just "getting older" symptoms? What if they're whispers of a deeper struggle? This is where the urgent screening part comes into play. We need to be more vigilant, more attuned to any subtle shift in behavior, any change in their vibrant personality. We must push past the societal tendency to brush off symptoms and accept that our elders are vulnerable, and their mental well-being is just as important as their physical health.
2. The Subtle Signals: Recognizing the Symptoms
Depression in seniors isn't always a dramatic, tearful affair. Sometimes it’s more like a slow, creeping fog. The symptoms can be as diverse as the individuals suffering from the illness. Let’s break down some of the most common red flags:
Persistent Sadness: This one’s pretty obvious, but sometimes it’s masked. Watch out for a general downcast mood, a lack of enthusiasm, or frequent expressions of feeling "empty" or "down."
Changes in Appetite and Weight: Are they eating significantly more or less than usual? Significant weight loss or gain can be a sign that something's amiss.
Sleep Disturbances: Difficulty sleeping, oversleeping (more than usual), or frequent waking during the night.
Loss of Interest in Activities: Are they no longer interested in hobbies they once loved? Do they avoid social gatherings or stop engaging in activities they used to find pleasurable?
Fatigue and Loss of Energy: Feeling tired all the time, even after getting a good night's sleep, is a major symptom.
Difficulty Concentrating: Trouble focusing, remembering things, or making decisions. Remember, this can sometimes be mistaken for dementia, so a proper diagnosis is key.
Physical Aches and Pains: Sometimes, depression can manifest as unexplained physical symptoms like headaches, stomach problems, or chronic pain.
Irritability and Agitation: Increased crankiness, impatience, or a quick temper.
Thoughts of Death or Suicide: This is a critical one. Any mention of wanting to die, feeling like life isn't worth living, or thoughts of self-harm should be taken very, very seriously.
3. Why Is Depression So Common in Seniors?
Let's be honest; aging itself can be a tough gig. Think about it: Loss of loved ones, declining health, financial worries, the feeling of losing independence, and social isolation. As we age, our lives undergo a variety of alterations. These transitions can feel incredibly heavy, akin to carrying a burdensome load. These factors alone create a fertile ground for depression to take root. Beyond these, other contributing causes include the physical changes to the brain as it ages, chronic illnesses, side effects of certain medications, and underlying genetic predispositions.
4. The Stigma Factor: Why Seniors May Hide Their Feelings
Nobody wants to feel like a burden. And seniors, especially, grew up in a time when mental health wasn't openly discussed. The stigma surrounding mental illness can be a huge barrier to seeking help. They might be embarrassed, ashamed, or afraid of being seen as "weak." They might also fear losing their independence if they admit to needing help. As a culture, we must champion empathy, and actively dismantle the stigma, creating an environment of trust and support where seniors can feel comfortable sharing their struggles.
5. The Importance of Early Detection: Why Screening Matters
Early detection of depression is paramount, like catching a fire before it devours a house. The sooner depression is diagnosed, the sooner treatment can begin, and the better the outcome will be. Untreated depression in seniors can lead to a host of serious consequences, including:
- Worsening physical health
- Increased risk of suicide
- Social isolation
- Impaired cognitive function
- Difficulty managing chronic illnesses
Regular screening can help identify depression early, before it spirals out of control.
6. Who Should Be Screened?
Honestly? Everyone. Especially if they exhibit any of the symptoms we mentioned earlier. Annual checkups, family conversations and even quick self-assessment questionnaires can be great starting points. Anyone experiencing changes in behavior, mood, or habits should be evaluated by a doctor or mental health professional.
7. Where Do You Start? The Screening Process
The initial step is to schedule an appointment with a primary care physician. They can perform a physical examination to rule out any underlying medical conditions contributing to the symptoms and can begin the screening process via a questionnaire, such as the Geriatric Depression Scale (GDS). If depression is suspected, the doctor will typically refer the individual to a mental health specialist for a more comprehensive evaluation. This may involve a detailed interview, a review of their medical history, and additional tests.
8. The Role of Family and Friends: Your Action Plan
You are the eyes and ears on the ground. You are the ones closest to your loved ones. Here’s how you can help:
- Educate Yourself: Learn about the symptoms of depression in seniors.
- Talk Openly: Create a safe space for your loved one to share their feelings. Listen without judgment. Use open-ended questions like, "How are you feeling today?" or "What's on your mind?" Instead of "Don't be sad," say "It's okay to feel sad."
- Offer Support: Let them know you’re there for them, and that you care. Offer practical help with daily tasks, appointments, and errands.
- Encourage Professional Help: Gently suggest that they speak with their doctor or a mental health professional.
- Be Patient: Treatment for depression takes time. There will be ups and downs. Be patient and supportive throughout the process.
- Take Care of Yourself: Supporting a loved one with depression can be emotionally draining. Make sure you're taking care of your own mental and physical health too.
9. Treatment Options: A Variety of Healing Pathways
The good news is that depression is highly treatable, and the options are as varied as the individuals experiencing the disease. These can include:
- Medication: Antidepressant medications can help regulate the brain's chemistry.
- Therapy: Talk therapy, such as cognitive behavioral therapy (CBT), can help change negative thinking patterns and behaviors.
- Support Groups: Connecting with others who understand what they're going through can be incredibly helpful.
- Lifestyle Changes: Regular exercise, a healthy diet, and sufficient sleep can greatly improve mood.
- Other Therapies: In some cases, other treatments like electroconvulsive therapy (ECT) may be considered.
10. Recognizing the Warning Signs: When to Seek Immediate Help
Some situations require immediate intervention. These might be considered red flags and will trigger an immediate response. If your loved one expresses thoughts of suicide, self-harm, or has a suicide plan, don't hesitate. Contact emergency services or take them to the nearest hospital immediately.
11. The Power of Positivity: Promoting Well-being and Resilience
While it’s important to address depression, we can also proactively nurture well-being in our seniors. Think of it like planting seeds to grow into sturdy plants. This includes:
- Encouraging Social Connections: Encourage them to stay connected with friends and family, join social groups, or volunteer.
- Promoting Physical Activity: Even short walks can make a difference.
- Encouraging Hobbies and Interests: Help them engage in activities they enjoy.
- Providing a Sense of Purpose: Encourage them to pursue meaningful activities, such as caring for grandchildren or volunteering.
- Creating a Supportive and Loving Environment: Surround them with love, compassion, and understanding.
12. Common Misconceptions About Depression in Seniors
Let's clear up a few myths:
- "Depression is a normal part of aging." Absolutely not. It’s a treatable illness.
- "Seniors are just being difficult." Depression can manifest as irritability and withdrawal, sometimes misconstrued as stubbornness.
- "They should just snap out of it." Depression is not a weakness or something that can be willed away.
- **"Medication is a sign of weakness."
Recommendations for Screening Older Patients for Depression

By Dr. Regina Koepp Recommendations for Screening Older Patients for Depression by Dr. Regina Koepp
Screening for Depression in Older Adults
By RCI Caregiving Screening for Depression in Older Adults by RCI Caregiving
SLUMS Examination & The Geriatric Depression Scale
By mmlearn.org SLUMS Examination & The Geriatric Depression Scale by mmlearn.org
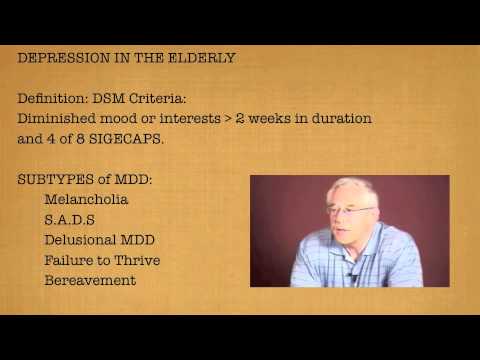
Title: Depression in the Elderly
Channel: mmlearn.org
Depression in the Elderly by mmlearn.org
Is THIS the SHOCKING Reason You're Depressed? (ICD-11 Criteria Revealed)
Is Your Elderly Loved One Hiding Depression? Urgent Screening Needed!
The golden years, a time often envisioned as one filled with contentment, relaxation, and the sweet reward of a life well-lived. Yet, for many seniors, this period is shadowed by a silent adversary: depression. Unlike the fleeting blues that may visit us all, clinical depression in the elderly isn't merely sadness; it's a complex and often debilitating illness that demands immediate attention. It is crucial to recognize the subtle, insidious ways depression can manifest in older adults, making the call for urgent screening paramount.
The Silent Scourge: Recognizing Depression in the Elderly
Depression in seniors, unlike the more stereotypical portrayals in younger populations, frequently presents differently. Instead of expressing overt sadness, older adults might exhibit a range of symptoms that are easily mistaken for other age-related issues. The key is to cultivate a keen awareness and observational finesse, detecting the nuanced signals that often precede a significant mental health crisis.
A Mask of Physical Ailments:
- Unexplained Physical Complaints: One of the most common disguises of depression is a barrage of physical ailments. Chronic pain that seems unresponsive to treatment, persistent fatigue, digestive issues without an apparent cause, and headaches can all be indicators of an underlying depressive disorder.
- Withdrawal from Social Activities: An abrupt cessation of participation in activities previously enjoyed, such as card games, club meetings, or gatherings with family and friends, warrants careful examination. Isolation, a hallmark of depression, can exacerbate feelings of loneliness and despair.
- Changes in Appetite and Sleep: Significant alterations in eating patterns, whether it’s a marked increase or decrease in food intake, should trigger concern. Similarly, disrupted sleep – insomnia or sleeping excessively – can be another red flag.
- Difficulties with Concentration and Memory: Cognitive difficulties, such as forgetfulness, trouble focusing, and experiencing problems with decision-making, can be attributed to many conditions, but they can also be attributed to depression. These changes can be dismissed as a normal part of aging, but they should not be ignored.
The Emotional Landscape: Unveiling Hidden Distress
Beyond the purely physical manifestations, understanding the shifts in an elderly individual's emotional state is critical. Here are some important emotional and behavioral aspects to observe that will increase the opportunities for a solution:
- Increased Irritability and Anger: Contrary to the romanticized notion of peaceful aging, some seniors experience heightened irritability, becoming easily angered and frustrated by situations that wouldn't have previously bothered them. This is a common reaction for persons who are suffering.
- Loss of Interest and Pleasure: Apathy, or a generalized lack of interest in activities and hobbies, signals a potential problem. If a senior derives no pleasure from their former interests, something is wrong.
- Feelings of Worthlessness and Hopelessness: These internal struggles are frequently voiced, even in a subdued manner. Phrases such as "What's the point?" or "Nobody cares" should never be dismissed as simple grumbling.
- Increased Talk of Death or Suicide: Any mention of death, suicide, or feeling like a burden is an immediate and urgent concern. It is critical to engage the necessary support and care immediately.
Factors That Increase the Risk of Depression in Seniors
Certain factors can render older adults more vulnerable to developing depression. Recognizing these risk factors allows for proactive monitoring and intervention.
- Chronic Illnesses and Pain: The burden of managing chronic health conditions, such as arthritis, heart disease, cancer, or diabetes, can significantly elevate the risk of depression. The physical limitations and emotional toll can be overwhelming.
- Loss and Grief: The aging process often involves facing multiple losses, including the passing of loved ones, friends, and spouses. The grieving process can be extremely challenging and lead to depressive symptoms.
- Social Isolation: Loneliness and social isolation are prevalent among older adults, especially those who live alone or have a limited social network. This lack of connection can exacerbate feelings of sadness and despair.
- Medication Side Effects: Certain medications can trigger and/or worsen depressive symptoms. It is essential to review a senior's medications regularly and consult with their physician about any potential side effects.
- Financial Difficulties: Financial strain can be a significant stressor for older adults, contributing to feelings of anxiety and helplessness. The worry of not being able to meet financial obligations can weigh heavily on their mental well-being.
The Critical Importance of Urgent Screening
Prompt screening for depression is not just a good idea; it is an imperative. Early detection opens the door to timely intervention and allows seniors to regain their vitality and quality of life.
- The Role of the Primary Care Physician: The primary care physician is often the first point of contact for seniors, making them ideally positioned to conduct screenings. Regular check-ups should include a simple, evidence-based screening tool for depression.
- The Value of Mental Health Professionals: If symptoms are suggestive of depression, assessment by a mental health professional, such as a psychiatrist, psychologist, or therapist, is essential. These professionals have the training and tools to diagnose and craft individualized treatment plans.
- The Benefits of Early Intervention: Early intervention can substantially improve outcomes. Treatment options may include psychotherapy (talk therapy), antidepressant medications, or a combination of both. Early treatment can make a drastic difference.
- Advocating for Your Loved One: Family members and friends play a vital role in advocating for the mental well-being of their elderly loved ones. This includes encouraging screening, supporting treatment plans, and providing a loving and understanding environment.
Creating a Supportive Environment: Helping Your Loved One Thrive
Beyond medical interventions, the surrounding environment plays a crucial role in a senior's mental health. Creating a supportive and nurturing environment is essential for their recovery and well-being.
- Empathy and Understanding: Listen to your loved one with empathy and strive to grasp their experiences. Let them know that their feelings are validated and that you are there for them.
- Encouraging Social Connection: Facilitate opportunities for social interaction, whether it's visiting friends and family, participating in group activities, or joining a club or organization. Social connection combats isolation.
- Promoting Physical Activity: Encourage gentle exercise, such as walking, swimming, or tai chi. If well, exercise boosts mood and provides physical benefits.
- Supporting Healthy Habits: Encourage a balanced diet, sufficient sleep, and moderate sun exposure. These habits help contribute to overall well-being.
- Seeking Professional Counseling: Consider supporting your loved one in therapy. If so, encourage the therapeutic process. Therapy is often used to give persons the tools to cope with depression.
- Patience and Persistence: Recovery from depression can be a gradual process. Practice patience and persistence, providing continuous support and encouragement throughout the journey.
The Takeaway: A Call to Action
If you are concerned about an elderly loved one, please remember that you are not alone. Depression is often hidden, but it is beatable. Recognize the signs, advocate for screening, support treatment, and provide unwavering love and support. The potential to restore joy, meaning, and vitality to the golden years makes this a mission worth pursuing.
