
Title: Pharmacology - Antidepressants - SSRI, MAOI, TCA, SNRIs nursing RN PN MADE EASY
Channel: SimpleNursing
Pharmacology - Antidepressants - SSRI, MAOI, TCA, SNRIs nursing RN PN MADE EASY by SimpleNursing
depression medication types, antidepressant medication types, depression treatment types, depression drug types, depression medication names, depression medication names list, depression medication names australia, depression medication names bupropion, depression medication names lexapro, depression medication categories
Escape the Darkness: Your Guide to Depression Medication Types
Breaking Through the Shadows: Navigating Depression Medication with Compassion
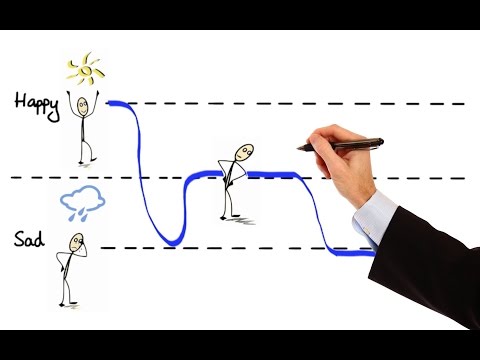
The weight of sadness. It can feel like an unseen hand, pulling you deeper. Dealing with depression is tough. It’s a journey, not a destination. Understand that you are not alone. Millions experience this every single day. Let's explore the tools available to help. Choosing the right path involves understanding your options.
Decoding the Landscape: Different Antidepressant Classes
Think of antidepressants as different keys. Each one unlocks a specific door. Knowing the various classes is the first step. These medications affect brain chemicals. They’re often referred to as neurotransmitters. Serotonin and norepinephrine are critical. These chemicals influence mood, sleep, and appetite. In addition, there's a range of classes to consider.
Selective Serotonin Reuptake Inhibitors (SSRIs): The Frontrunners
SSRIs are often the initial go-to. They’re generally well-tolerated. Their primary mechanism is simple. They increase serotonin levels in the brain. As a result, this can improve mood regulation. Common examples include fluoxetine and sertraline. Furthermore, SSRIs can address anxiety too. Keep in mind that side effects vary. Every individual responds differently. Consequently, consult with your doctor.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): A Dual Approach
SNRIs take a broader approach. They target both serotonin and norepinephrine. This dual action can be beneficial. They can be effective for pain management. Besides, they also help manage depression. Venlafaxine and duloxetine are examples. Therefore, they are chosen for certain patients. However, side effects can demand careful monitoring.
Tricyclic Antidepressants (TCAs): A Time-Tested Option
TCAs have been around for a while. They work by influencing multiple neurotransmitters. They can be very effective. However, they often have more side effects. Although they are still used today, they aren't a first choice. Amitriptyline and nortriptyline are examples. Because of the potential side effects, doses must be carefully controlled. For those who respond, they can be a lifesaver.
Monoamine Oxidase Inhibitors (MAOIs): A More Specific Path
MAOIs are another older class. They work by inhibiting an enzyme. This enzyme breaks down neurotransmitters. In this case, it can increase availability. They are often reserved for specific situations. Dietary restrictions are required while taking MAOIs. On the other hand, they can be incredibly effective. For instance, they can help with treatment-resistant depression.
Atypical Antidepressants: Exploring Unique Opportunities
This group is quite varied. Indeed, they don’t fit neatly into other categories. Bupropion, for example, affects dopamine. Mirtazapine influences several systems. Furthermore, these medications offer diverse benefits. They can address different symptoms. They can also impact quality of life. Having said that, they require careful consideration.
Beyond the Pill: Complementary Therapies
Medication is often only part of the solution. Therapy is a critical component. Cognitive Behavioral Therapy (CBT) is quite effective. It allows you to change negative thought patterns. Exercise and a healthy diet provide support. Likewise, mindfulness and meditation can help. In addition, support groups can build a community.
The Medication Journey: Expectations and Adjustments
Finding the right medication takes time. It’s not an instant fix. In essence, it is trial and error. Be patient with the process. You can expect to see results over weeks. Also, side effects can be managed. Communication with your doctor is essential. You may need to adjust the dose. Moreover, you may try a different medication altogether.
Working with Your Care Team: Open Communication
Your doctor is your partner. Be honest about your symptoms. Describe any side effects comprehensively. As a result, your doctor can help you adjust. Psychiatrists specialize in mental health. Therapists offer valuable support. Family and friends can also provide support. Consequently, build a support system.
Embracing the Future: Hope and Healing
You deserve to feel better. Recovery is possible. Therefore, take the first step today. Seek professional help and start talking. Don’t give up on yourself. Finally, it’s a journey worth taking. You can break through the darkness.
Anxiety Meltdown? Tart Cherries Could Be Your Secret Weapon!Escape the Darkness: Your Guide to Depression Medication Types
Alright, friends, let's have a real talk. We all know the struggle. That heavy cloak of shadows, that overwhelming feeling of… well, just blah. Depression. It’s a thief, stealing joy, motivation, and often, our very sense of self. And let's be honest, finding your way out of that darkness can feel like navigating a labyrinth blindfolded. But, take a deep breath. We're in this together. This isn’t a lecture; it’s a conversation about one of the most crucial tools in your escape kit: depression medication.
1. Why This Matters: Understanding the Battle
Before we dive into the specifics, let's acknowledge the elephant in the room: there's STILL a stigma around mental health. Talking about medication? Even more so. But listen, just like someone with diabetes needs insulin, someone battling depression might need medication to help rebalance the chemicals in their brain. It's about taking care of you. It’s about fighting back. It’s about reclaiming your life. This guide is for you, the warrior, the survivor, the one ready to take back control.
2. The Brain Boogie: What's Actually Happening?
Think of your brain as a bustling city. Signals, thoughts, and emotions are constantly zipping around, carried by tiny couriers called neurotransmitters. When those couriers aren't delivering the goods properly, things can go sideways. Depression often involves imbalances in these neurotransmitters, particularly serotonin, norepinephrine, and dopamine. Medications work their magic by helping to regulate these delicate chemical messengers. It's like fine-tuning the radio to get the right signal.
3. Selective Serotonin Reuptake Inhibitors (SSRIs): The Front Line Fighters
Think of SSRIs as the first line of defense. They’re like the bouncers at a club, ensuring serotonin stays around longer in the party zone of your brain. By preventing the reabsorption (reuptake) of serotonin, SSRIs make more of it available to do its job. Common examples include fluoxetine (Prozac), sertraline (Zoloft), and paroxetine (Paxil). They can be super effective, but also come with potential side effects. Side effects, like anything, can differ from person to person; some people don't experience them at all!
4. Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): The Double Duty Heroes
SNRIs are the power couple of the neurotransmitter world. They not only boost serotonin but also norepinephrine, which plays a role in mood and alertness. Think of them as the all-stars. Venlafaxine (Effexor) and duloxetine (Cymbalta) are popular SNRI options. They can be effective for both depression and physical pain. As always, side effects are possible, so it's important to discuss them with your doctor.
5. Tricyclic Antidepressants (TCAs): The Old Guard
TCAs were some of the first medications used to treat depression. They work by blocking the reabsorption of serotonin and norepinephrine. However, they often come with more side effects than newer medications and can be dangerous in overdose. Because of this, they’re usually reserved for those who haven’t found relief with other options. It's like the classic car in the garage, reliable but requires careful handling.
6. Monoamine Oxidase Inhibitors (MAOIs): The Special Ops Team
MAOIs are a specific type of antidepressant that were the first developed. They work by blocking an enzyme called monoamine oxidase, which breaks down neurotransmitters. They can be very effective but require strict dietary restrictions (no aged cheeses, cured meats, etc.) and can interact with other medications. They're like the highly trained specialists, offering a unique approach, but demanding careful consideration.
7. Atypical Antidepressants: The Wild Cards
This category includes medications that don't quite fit into the other groups. They have different mechanisms of action, but are all dedicated to easing depressive symptoms. Bupropion (Wellbutrin), for example, works mainly on dopamine and norepinephrine, is often used to help with smoking cessation, and doesn’t typically cause the sexual side effects sometimes associated with SSRIs. Mirtazapine (Remeron) works on multiple receptors and can sometimes help with sleep and appetite. These are like the secret weapons.
8. The Side Effect Symphony: What to Expect (and What Not To)
No medication is perfect. Side effects are, unfortunately, a potential part of the journey. The most common? Nausea, sleep disturbances, weight changes, and sexual dysfunction. The key is communication! Tell your doctor everything. Don’t be shy. Think of it like tuning an instrument; some adjustments might be needed to get that perfect sound. Often, side effects will diminish over time, but don’t hesitate to make sure you are getting the most out of your medicine.
9. Finding the Right Fit: It’s a Marathon, Not a Sprint
Finding the "right" medication is a process, often involving trial and error. It's like choosing the perfect pair of shoes. What works for one person might not work for another. Your doctor will assess your symptoms, medical history, and other medications you’re taking to help you figure out what might be best. Be patient with yourself, and don't give up.
10. Dosage Diary: The Importance of Following Instructions
Follow your doctor's instructions exactly. Don’t skip doses. Don’t double up. Keep a journal, track your symptoms and how you feel. This information will be incredibly helpful for your doctor in assessing your progress and making any necessary adjustments to the dosage.
11. Time to Bloom: How Long Does It Take to See Results?
Antidepressants aren't instant fixes. They typically take 4-6 weeks to reach their full effect. This is where patience is crucial. It's like planting a seed; you have to water it and give it sunlight, and it takes time for it to grow. Don't give up before you see the progress.
12. The Power of Combo: Therapy and Medication – The Ultimate Duo
Medication is often most effective when combined with therapy. Think of it as having a supporting player in your journey to wellness. Therapy provides you with the tools and strategies to manage your thoughts, feelings, and behaviors. Together, medication and therapy pack a real punch.
13. Lifestyle Boosters: How to Support Your Healing
Medication is not a magic bullet. Nourishing your body and mind can significantly improve your experience. Regular exercise, a healthy diet, adequate sleep, and stress-management techniques (like meditation or mindfulness) can all make a huge difference. These actions are the supporting cast to the main characters of your recovery journey.
14. When to Seek More Help: Knowing the Red Flags
If you're experiencing worsening symptoms, thoughts of self-harm, or severe side effects, don't hesitate to reach out. Contact your doctor or find the nearest emergency room immediately. You are not alone, and help is always available.
15. Tapering Off: Doing It Right, Safely
Never stop taking your medication without consulting your doctor. Abruptly stopping can cause withdrawal symptoms. Your doctor will guide you through a gradual tapering-off process, ensuring your safety and well-being.
Closing Thoughts: You Are Unbreakable
We’ve covered a lot, haven’t we? From the chemical dance in your brain to the different types of medications available. Remember, this isn’t a solo mission. Reach out to your doctor, your therapist, your support network. You deserve a life filled with sunshine, laughter, and joy. You are stronger than you think. You are resilient. You are capable of healing. And we're here to walk alongside you on this journey.
FAQs: Your Questions Answered
FAQ 1: Will I be on medication forever?
Not necessarily. Some people require long-term medication, while others can eventually taper off under the guidance of their doctor once their symptoms are well-managed. It really depends on the individual.
FAQ 2: What if I don't like the side effects?
Talk to your doctor! They might be able to adjust your dosage, switch medications, or recommend strategies to manage the side effects. Don't suffer in silence.
FAQ 3: Is it possible to overdose on antidepressants?
Yes, it's possible, especially with older antidepressants like TCAs. Always take your medication as prescribed, and keep them safely out of reach of children.
FAQ 4: Can antidepressants make me gain weight?
Some antidepressants can cause weight gain, while others might lead to weight loss. Talk to your doctor about your concerns and how to manage any weight changes.
FAQ 5: Can I drink alcohol while taking antidepressants?
It's generally not recommended to drink alcohol while taking antidepressants, as it can worsen side effects and interfere with the medication's effectiveness. Talk to your doctor about any potential interactions.
1) Principal Keywords: Depression Meds, Medication Guide 2) SEO Headline: Depression Meds: Your Guide to Medication Types 3) Pathway: Meds Guide 4) Meta Summary: Fighting depression? Learn about the different types of depression medications with our comprehensive guide. Find the right fit and start your journey to wellness. 5) Image Alt Text: A
Heartbreak Hotel: The Saddest Urdu Love Quotes You'll Ever ReadPharmacology - Antidepressants, Animation

By Alila Medical Media Pharmacology - Antidepressants, Animation by Alila Medical Media
How do antidepressants work - Neil R. Jeyasingam

By TED-Ed How do antidepressants work - Neil R. Jeyasingam by TED-Ed
Major Depression and SSRI'sSNRI's

By Dirty Medicine Major Depression and SSRI'sSNRI's by Dirty Medicine
Title: Pharmacology - ANTIDEPRESSANTS - SSRIs, SNRIs, TCAs, MAOIs, Lithium MADE EASY
Channel: Speed Pharmacology
Pharmacology - ANTIDEPRESSANTS - SSRIs, SNRIs, TCAs, MAOIs, Lithium MADE EASY by Speed Pharmacology
This Depression Test Will SHOCK You (And Help You Get Better)
Escape the Darkness: Your Guide to Depression Medication Types
Navigating the landscape of depression can feel overwhelming. The struggles are real, the emotions complex, and finding the right path to wellness requires understanding and support. For countless individuals, medication becomes a crucial component of that journey, offering a beacon of hope amidst the shadows. We are dedicated to providing you with a comprehensive overview of the most common types of depression medication, empowering you with the knowledge you need to have informed conversations with your healthcare provider and actively participate in your own healing process. This guide isn't a replacement for professional medical advice – it's a starting point. It’s a resource, designed to illuminate the options available and foster a sense of clarity.
Selective Serotonin Reuptake Inhibitors (SSRIs): The Frontline Fighters
Selective Serotonin Reuptake Inhibitors (SSRIs) represent a widely prescribed class of antidepressants, frequently considered the first line of defense in treating depression. They operate by selectively targeting serotonin, a neurotransmitter integral to mood regulation. Serotonin, often associated with feelings of well-being and happiness, plays a crucial role in brain function. SSRIs work by preventing the reabsorption (reuptake) of serotonin in the brain. This process allows more serotonin to be available, leading to improved mood and a reduction in depressive symptoms.
Specific examples of SSRIs include fluoxetine (Prozac), sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), and escitalopram (Lexapro). Each medication possesses a slightly different chemical structure, potentially influencing how individuals experience its effects. Factors like metabolism, specific receptor interactions, and other individual biochemical variations contribute to the unique response people will have to these medications.
The benefits of SSRIs often include improved mood, reduced anxiety, enhanced sleep quality, and increased energy levels. It's important to realize that these effects don't always manifest immediately. It usually takes several weeks, sometimes even longer, for the full therapeutic impact to become apparent. During this initial adjustment period, some individuals may experience side effects, such as nausea, insomnia, changes in weight, or sexual dysfunction. These side effects are generally temporary, and often subside as the body adjusts to the medication. Open communication with your healthcare provider is paramount during this phase. They are adept at addressing any concerns and can potentially adjust dosages or provide strategies to alleviate side effects.
Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs): Double-Duty Relief
Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs) represent another common class of antidepressants. These drugs work by inhibiting the reuptake of both serotonin and norepinephrine, two essential neurotransmitters. While serotonin primarily impacts mood, norepinephrine plays a significant role in attention, alertness, and energy levels. SNRIs are particularly effective for individuals experiencing depression accompanied by fatigue, lack of concentration, or chronic pain.
Commonly prescribed SNRIs include venlafaxine (Effexor), duloxetine (Cymbalta), and desvenlafaxine (Pristiq). Like SSRIs, SNRIs require time to achieve their full effect. The impact on mood, energy, and focus may become apparent within a few weeks of consistent use.
Side effects are possible and can be similar to those associated with SSRIs. This includes nausea, insomnia, changes in appetite, and changes in sexual function. Some individuals may experience increased blood pressure or heart rate. Close monitoring and open communication with your healthcare provider are essential, particularly if you have pre-existing health conditions. They can monitor these vital signs and make the adjustments to minimize adverse effects and maximize treatment efficacy.
Tricyclic Antidepressants (TCAs): Older, Yet Relevant
Tricyclic Antidepressants (TCAs) represent an older class of antidepressants and were originally developed to treat a variety of mental health conditions. TCAs work by blocking the reuptake of both serotonin and norepinephrine, similar to SNRIs, and they also affect other neurotransmitter systems. While less frequently prescribed today due to their higher potential for side effects compared to newer medications, TCAs remain a viable option, particularly for individuals who haven't found relief from other treatments.
Examples of TCAs comprise amitriptyline, imipramine, nortriptyline, and desipramine. TCAs can be quite effective, frequently alleviating the symptoms of depression, and can also provide relief from chronic pain and neuropathy.
Due to their potential for more serious side effects, TCAs require careful monitoring. Common side effects include dry mouth, blurred vision, constipation, drowsiness, and weight gain. TCAs also have the potential to cause cardiac side effects, so a baseline electrocardiogram (EKG) may be required before initiating treatment, particularly in individuals with pre-existing heart conditions. Dosage adjustments and ongoing monitoring by your healthcare provider are essential to ensure safety and effectiveness.
Monoamine Oxidase Inhibitors (MAOIs): A Specialized Approach
Monoamine Oxidase Inhibitors (MAOIs) represent a distinct class of antidepressants that operate by inhibiting the enzyme monoamine oxidase. This enzyme is responsible for breaking down neurotransmitters like serotonin, norepinephrine, and dopamine. By inhibiting MAO, these medications increase the availability of these neurotransmitters in the brain. MAOIs are typically reserved for cases of depression that haven't responded to other treatments due to their potential for serious interactions with certain foods and medications.
Commonly prescribed MAOIs comprise phenelzine (Nardil), tranylcypromine (Parnate), and isocarboxazid (Marplan). MAOIs can demonstrate efficacy in treating treatment-resistant depression, and have been shown to be effective in managing certain types of anxiety disorders.
The primary concern associated with MAOIs is their interaction with tyramine, a substance found in certain foods like aged cheeses, cured meats, and fermented products. Consuming these foods while taking an MAOI can lead to a dangerous increase in blood pressure, known as a hypertensive crisis. Additionally, MAOIs can interact negatively with other medications, including certain other antidepressants, decongestants, and some herbal supplements. Strict adherence to dietary guidelines and medication precautions is crucial for safety when taking MAOIs. Treatment with MAOIs requires close supervision by a healthcare professional to ensure proper medication management and mitigate the risk of adverse interactions.
Atypical Antidepressants: Targeting Specific Needs
The term "atypical antidepressants" encompasses a group of medications that don't readily fit into the other categories. These drugs possess unique mechanisms of action and are often used to address specific aspects of depressive symptoms or to treat individuals who can't tolerate or haven't responded to other types of antidepressants.
Examples of atypical antidepressants include bupropion (Wellbutrin), mirtazapine (Remeron), trazodone (Desyrel), and vilazodone (Viibryd). Bupropion primarily affects dopamine and norepinephrine, often used to treat depression and aid in smoking cessation. Mirtazapine acts on serotonin and histamine receptors, helping with depression, anxiety, and sleep difficulties. Trazodone primarily affects serotonin, commonly prescribed for insomnia and depression. Vilazodone works by inhibiting serotonin reuptake and acting as a partial agonist at the 5-HT1A receptor.
The side effects associated with atypical antidepressants vary depending on the specific medication. Some possible side effects include insomnia, agitation, dry mouth, and sexual dysfunction. The choice of atypical antidepressants is based on an assessment of individual symptoms, other medical conditions, and medication interactions. Close communication with the physician is essential to determine the most suitable treatment option.
Understanding the Nuances: Beyond Medication
It is critical to understand that medication is often just one component of a comprehensive treatment plan for depression. While medication can be profoundly helpful in regulating mood and reducing symptoms, it's frequently most effective when combined with other therapies.
Psychotherapy, particularly cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT), can provide patients with a wide range of tools and strategies to manage their thoughts, emotions, and behaviors. CBT can help identify and replace negative thought patterns. IPT can help improve interpersonal relationships, which can be a source of stress for individuals.
Lifestyle adjustments can also play a crucial role in managing depression. Regular exercise, a balanced diet, sufficient sleep, and stress-reduction techniques can significantly improve mental well-being. Engaging in social activities, connecting with supportive friends and family, and participating in hobbies and interests can also foster a sense of connection and purpose.
Working with Your Healthcare Provider: A Partnership for Healing
Choosing the right medication, and developing a successful treatment plan, is a highly personal process. It involves a collaborative approach between you and your healthcare provider, usually a psychiatrist or a primary care physician. During your initial consultation, be prepared to share a thorough medical history, describing your symptoms, their duration, and any factors that might be triggering them. Be open about any other medical conditions you have and any medications, supplements, or other substances you're taking.
Your healthcare provider will evaluate your symptoms and medical history and then discuss the potential benefits and risks of different antidepressant medications. They will also consider factors, such as any previous responses to medications, other health conditions, and potential for drug interactions. Don't hesitate to ask questions about the medication, including how it works, potential side effects, and how long it might take to be effective.
It is important to stay in regular contact with your healthcare provider during treatment. They will monitor your progress, assess side effects, and make adjustments to your medication as needed. Do not stop taking your medication or change your dosage without first consulting your doctor, even if you feel better.
The journey to recovery from depression is unique for each individual. By understanding the different types of depression medication, and by engaging in open communication with your healthcare provider, you can begin to navigate this path with greater confidence and hope.
