
Title: Bipolar disorder depression & mania - causes, symptoms, treatment & pathology
Channel: Osmosis from Elsevier
Bipolar disorder depression & mania - causes, symptoms, treatment & pathology by Osmosis from Elsevier
bipolar major depression icd 10, bipolar severe depression icd 10, bipolar disorder severe depression icd 10, icd 10 code for major depression with bipolar disorder, mdd with bipolar icd 10
Bipolar Depression ICD-10: The Shocking Truth Doctors Don't Want You to Know
Unmasking the Shadows: Navigating the Unseen Realities of Bipolar Depression
Hey there, friend. Ever feel like you're riding a relentless emotional rollercoaster? This wild ride might be more than just a bad day. It could be something deeper. We're talking about bipolar depression and the sometimes-hidden truths surrounding it. Let’s unpack this together.
Decoding the Code: Bipolar Depression and the ICD-10
Firstly, let us address the elephant in the room: the ICD-10. This is the International Classification of Diseases, Tenth Revision. It’s a globally recognized system. It helps doctors and researchers. The ICD-10 codes classify diseases and conditions. It's the diagnostic bible, essentially. Bipolar depression falls under this system. This is how professionals understand and document the illness. Knowing the code is helpful. However, it does not define the individual's journey.
Beyond the Diagnosis: The Lived Experience
Secondly, let's be incredibly clear. A diagnosis is just the beginning. Bipolar depression is not a monolith. People experience it differently. The "shocking truth" isn’t a secret conspiracy. It's acknowledging the individual human experience. It acknowledges all the nuances. Symptoms fluctuate dramatically. At times, it feels like a constant battle. Recovery also looks different for each person.
The Rollercoaster Effect: Mood Swings and Their Impact
Then, consider the mood swings. We’re talking about extreme shifts. These impact everything. From your sleep to your energy levels. Your decision-making is also affected. Highs and lows are characteristic of bipolar disorder. This is the very essence of managing the process. These swings impact everything. They can create significant disruptions. It isn't just feeling "sad" or "happy." It's a complete overhaul.
The Hidden Struggles: Challenges You Might Face
Furthermore, there are often hidden struggles. These are often overlooked. Stigma is a huge hurdle. Many people still don't understand mental illness. Therefore, they may judge you. Finding the right treatment can be tricky. It is not always a simple process. Access to mental health care is inconsistent. Insurance coverage can be a barrier. The impact on relationships is another challenge. Family and friends may struggle. They might not know how to help. This is another reality.
Treating the Whole Person: A Holistic Approach
Moreover, effective treatment requires a holistic approach. Remember, this is a complex condition. Medications are often necessary. They help stabilize mood. Therapy is a key component. Cognitive Behavioral Therapy (CBT) offers tools. These tools can manage thoughts and behaviors. Lifestyle changes are also crucial. Sleep, diet, and exercise matter. Support groups provide invaluable connections. They offer shared experiences. Finding the right combination takes time. It can be a process of trial and error.
The Importance of Self-Advocacy: Your Voice Matters
Plus, self-advocacy is vital. You are the expert on your own experience. Speak up about your needs. Voice your concerns to your doctor. Educate yourself about your condition. Join support groups and connect with others. Learn to recognize your triggers. Have a plan for when you’re struggling. Don’t be afraid to seek help. It's important to have a support network.
Dispelling Myths: What You Need to Know
However, let's banish some myths. Bipolar depression is not a personal failure. It is a medical condition. It doesn't mean you're "crazy" or "weak." Recovery is possible. People can and do live fulfilling lives. Proper treatment and support are crucial aspects. Do not give up hope. You are not alone in this fight.
Finding Strength: Embracing Your Journey
Finally, remember your strength. Living with bipolar depression is a challenge. It can be a difficult journey. You are resilient. You are capable of managing your condition. Celebrate your small victories. Focus on your well-being. Practice self-compassion. Allow yourself to be kind to yourself. Embrace the challenges. You can absolutely thrive. Take it one day at a time. Your journey is unique. Embrace your power.
Bipolar Depression: The Shocking Truth Doctors Don't Want You to KnowBipolar Depression ICD-10: The Shocking Truth Doctors Don't Want You to Know
Hey there, everyone! Ever feel like you're on a rollercoaster, only the track is made of quicksand? That, my friends, is a pretty accurate analogy for living with bipolar disorder, specifically the rollercoaster dip known as bipolar depression. We're going to dive deep today, beyond the surface level, and uncover some of the truths surrounding this often-misunderstood condition, specifically when it comes to the diagnostic code ICD-10. Let's be honest, some of the info out there feels like it's whispered in hushed tones, doesn’t it? We're going to shine a spotlight on it.
1. What Is Bipolar Depression Anyway? Decoding the Mystery
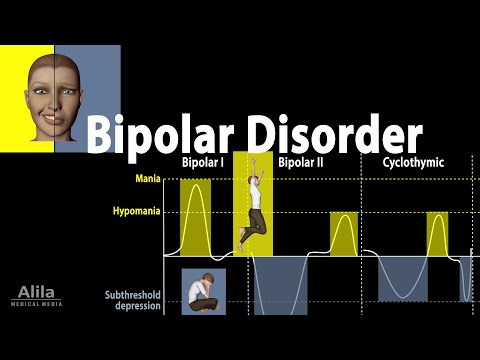
Okay, let's start with the basics. Bipolar depression isn't just feeling "down" for a few days. It’s a significant mood disorder characterized by intense shifts in mood, energy, and activity levels. We're talking about episodes of extreme sadness, hopelessness, and loss of interest in activities we usually enjoy, often coinciding with periods of elevated mood (mania or hypomania). Think of it like this: imagine your emotions as a spectrum. On one end, you have crippling depression; on the other, you have manic highs. The ICD-10 (International Classification of Diseases, 10th Revision) is a system used by doctors to diagnose and classify different medical conditions, including bipolar disorder. Understanding the different types (Bipolar I, Bipolar II, Cyclothymic Disorder) is the first step.
2. The ICD-10 Code: Why Does It Matter?
Why are we focusing on the ICD-10 code? Because it's the official language doctors use when diagnosing and treating bipolar depression. It’s how your condition is logged (F30-F39, which covers mood (affective) disorders), and it influences your treatment plan, insurance coverage, and access to resources. This is the bureaucratic backbone of mental health, but it's crucial to grasp its significance. It acts like a key unlocking the door to understanding your illness.
3. The "Shocking" Element: The Hidden Nuances of Diagnosis
Now, the juicy stuff. What's the "shocking" truth? Well, It’s not necessarily a conspiracy, but the complexities of diagnosis can be… interesting. The symptoms of bipolar depression can often mimic other conditions like major depressive disorder. This can lead to misdiagnosis and, consequently, ineffective treatment. Getting it right is the ultimate goal, right?
4. Misdiagnosis: When the Tracks Go Wrong
Misdiagnosis is a huge issue. Imagine trying to put a puzzle together with the wrong pieces. That's what happens when someone's bipolar depression is mistaken for something else. Sometimes, a doctor might only see the depressive episodes and prescribe antidepressants, which can actually worsen the condition if the patient is also experiencing undiagnosed mania. It’s like trying to put out a fire with gasoline!
5. The Antidepressant Dilemma: Fueling the Fire?
Here's the kicker: antidepressants, while often helpful for major depressive disorder, can trigger manic episodes in people with undiagnosed bipolar disorder. This means what might initially seem like relief could quickly spiral into a dangerous cycle of highs and lows. We’ll talk about the potential for "bipolar switching" (moving from depression to mania) later.
6. Unmasking Bipolar II: The Subtle Rollercoaster
Bipolar II is the stealthy sibling of Bipolar I. It's defined by depressive episodes and hypomanic episodes (less intense than mania). It’s often harder to spot because the hypomanic periods might seem like high energy, productivity, or creativity – until they crash. Think of it as feeling slightly above average, then falling off a cliff.
7. The Role of Genetics and Family History
Let's be real: mental health isn't always a solo act. It's worth noting the role genetics and family history play in the development of bipolar disorder. If you have a family member with bipolar disorder, your risk increases. It doesn't guarantee you'll develop it, but it's an important piece of the puzzle.
8. Unpacking the Symptoms: Beyond Sadness
Bipolar depression isn't just about feeling sad. The symptoms can include:
- Persistent sadness, anxiety, or emptiness
- Loss of interest in activities
- Fatigue or loss of energy
- Changes in appetite or sleep
- Feelings of worthlessness or guilt
- Difficulty concentrating
- Thoughts of death or suicide.
Sometimes it feels like more than a heavy weight; it's an all-consuming vortex.
9. The Manic/Hypomanic Side: The Flip Side of the Coin
It’s important to remember there’s another side to the coin. Although we're focusing on the depression piece, understanding the manic and hypomanic episodes is key to a proper diagnosis. Mania could manifest as extremely elevated mood, racing thoughts, increased energy, reckless behavior, and impulsivity. Hypomania is a less intense version of this.
10. The Diagnostic Process: What to Expect
Getting a diagnosis isn't always a quick fix. It often involves:
- A thorough medical history and physical exam
- A detailed discussion of your symptoms
- A psychological evaluation
- Possibly, a mood chart or diary to track your experiences.
Don't be afraid to ask questions, and be honest with your healthcare professional!
11. Treatment Options: Finding the right Combo
Treatment for bipolar depression is usually a combination of medication and therapy. Common approaches include:
- Mood stabilizers: (Lithium, lamotrigine, etc.) to manage mood swings.
- Antidepressants: (Use cautiously, often in conjunction with mood stabilizers).
- Antipsychotics: (Sometimes used short-term to manage severe mania or depression).
- Psychotherapy: (Cognitive Behavioral Therapy (CBT), interpersonal therapy, etc.) to help you cope and develop healthy coping strategies.
Finding the right combination might take time and adjustments.
12. The Stigma Factor: Speaking Up and Seeking Help
Let’s talk stigma. Unfortunately, there's still a stigma surrounding mental illness. It can make people hesitant to seek help or talk openly about their experiences. This needs to change, and it starts with us! Remember, you're not alone.
13. Self-Care Strategies: Your Daily Toolkit
Living with bipolar depression requires a conscious effort towards self-care. This includes:
- Establishing a regular sleep schedule
- Engaging in regular exercise
- Eating a balanced diet
- Avoiding alcohol and drugs (which can worsen symptoms)
- Practicing mindfulness techniques
- Building a strong support system.
Think of them as your personal safety nets.
14. Navigating Relationships: Support Systems are Vital
Bipolar disorder can impact relationships. Open communication, patience, and understanding are paramount. Educate your loved ones, set boundaries, and encourage them to seek support for themselves. Surrounding yourself with supportive people is like having a shield against the storm.
15. The Future of Bipolar Depression: The Road Ahead
Research into bipolar disorder is always evolving. We're continually learning more about its causes, developing new treatments, and improving diagnostic accuracy. We can expect further research, enhanced therapeutic strategies, and advancements in personalized medicine that can tailor treatment to the unique needs of each individual.
Closing Thoughts: You Are Not Defined by Your Diagnosis
We've covered a lot of ground today. Bipolar depression is a complex, often challenging condition, but it's also manageable. Remember that you are not defined by your diagnosis. Recovery is possible, and a fulfilling life is within reach. The journey may not always be easy, but it's worth it. Keep educating yourself, seek help when needed, and never give up on yourself. You've got this!
FAQs:
- Is bipolar disorder curable? Currently, there isn’t a cure, but it is highly treatable. With the right treatment plan and support, many people with bipolar disorder live full and productive lives.
- What should I do if I think I have bipolar disorder? Talk to your doctor or a mental health professional. They can conduct a thorough evaluation and help you get the right diagnosis and treatment.
- Can I take antidepressants if I have bipolar depression? This depends. Sometimes antidepressants are used, but they must be prescribed and monitored very carefully, usually in combination with a mood stabilizer. Incorrect use can worsen symptoms.
- How can I support someone with bipolar disorder? Educate yourself about the condition, be patient, offer support, and encourage them to seek professional help.
- Where can I find more resources and support? The internet is a good place to start. Search for reputable organizations and mental health resources.
1) Principal Keywords: Bipolar Depression ICD-10 Treatment 2) SEO Headline: Bipolar Depression: ICD-10 Secrets & Effective Treatments 3) Pathway: BipolarTreatment 4) Meta Summary: Facing Bipolar Depression? Learn the truth behind ICD-10 codes, treatment options, & secrets doctors may not tell you. 5) Image Alt Text:
Is This Depression? SHOCKING Quiz Reveals ALL (PDF Inside)Major Depressive Disorder MDD - Psychiatric Mental Health LevelUpRN

By Level Up RN Major Depressive Disorder MDD - Psychiatric Mental Health LevelUpRN by Level Up RN
Bipolar Affective Disorder CAUSES, SYMPTOMS, ICD-10 CRITERIA & MANAGEMENT

By Medicine Made Simple Bipolar Affective Disorder CAUSES, SYMPTOMS, ICD-10 CRITERIA & MANAGEMENT by Medicine Made Simple
Bipolar Disorder Symptoms, Risk Factors, Causes, Diagnosis and Treatments, Animation
By Alila Medical Media Bipolar Disorder Symptoms, Risk Factors, Causes, Diagnosis and Treatments, Animation by Alila Medical Media

Title: Depression CAUSES, SYMPTOMS, ICD-10 CRITERIA & MANAGEMENT
Channel: Medicine Made Simple
Depression CAUSES, SYMPTOMS, ICD-10 CRITERIA & MANAGEMENT by Medicine Made Simple
Escape the Darkness: Healthy Ways to Conquer Depression
Bipolar Depression ICD-10: The Shocking Truth Doctors Don't Want You to Know
The shadows of mood disorders, particularly those encompassing the complex interplay of bipolar disorder and depressive episodes, often cast a long shadow. They infiltrate every facet of life, from the simplest daily routines to profound, life-altering decisions. Examining the ICD-10 classification, the standard diagnostic framework used by medical professionals globally, reveals a detailed, yet often misunderstood, picture of this intricate condition. We embark on a journey to uncover the less-spoken truths surrounding bipolar depression, offering a perspective that transcends the ordinary.
Decoding the ICD-10: A Foundation for Understanding
The International Classification of Diseases, Tenth Revision (ICD-10), a widely utilized resource, acts as the bedrock for diagnosing and classifying diseases, including mental health disorders. Within this system, bipolar disorder is meticulously categorized, with specific codes assigned to various subtypes and episodes. The ICD-10 facilitates a common language among healthcare providers, offering a structured method for documentation and the precise tracking of patient conditions. Understanding the codes is crucial to grasping the nuances of diagnosis and treatment. Navigating this system can be like deciphering an ancient map, revealing the hidden pathways of the human psyche.
The Subtle Differences: Differentiating Bipolar Depression from Unipolar Depression
One of the most challenging aspects of bipolar disorder is distinguishing its depressive episodes from those associated with unipolar depression. The diagnostic process relies heavily on the patient's history, the presence of specific symptoms, and often necessitates a period of careful observation. A key differentiator is the existence of manic or hypomanic episodes. These periods of elevated mood, increased energy, and often erratic behavior, are the hallmarks of bipolar disorder. Their presence, even if brief or subtle, is a critical indicator. The distinction is more than mere semantics; it governs the type of treatment administered, including medication and therapeutic interventions. Misdiagnosis can lead to ineffective treatment and undue suffering.
Beyond the Blues: The Spectrum of Bipolar Disorder
Bipolar disorder is not a monolithic entity. The condition exists along a spectrum, ranging from Bipolar I to Bipolar II, and other specified and unspecified bipolar and related disorders. Bipolar I is defined by the presence of manic episodes that may or may not be accompanied by depressive episodes. Bipolar II, on the other hand, is characterized by depressive episodes coupled with hypomanic episodes, which are less severe than full-blown mania. The spectrum extends to include cyclothymic disorder, a milder form of bipolar disorder, characterized by fluctuations between hypomanic and depressive symptoms that do not meet the criteria for full-blown episodes. Each subtype presents its unique set of challenges, requiring a tailored approach to treatment and care. The spectrum's breadth underscores the importance of personalized care.
The Hidden Struggles: The Impact of Bipolar Depression
The impact of bipolar depression extends far beyond the confines of mood. This condition can substantially impair every aspect of life. The emotional toll is heavy, leading to profound sadness, hopelessness, and loss of interest in activities once enjoyed. Cognitive functions, such as concentration and memory, can become impaired, impacting work performance, relationships, and overall well-being. Physical symptoms, including fatigue, sleep disturbances, and changes in appetite, further compound the suffering. The risk of suicidal ideation and attempts is elevated, highlighting the urgency of timely diagnosis and intervention. The insidious nature of bipolar depression demands our unwavering attention.
Navigating the Diagnostic Maze: The Role of Thorough Evaluation
Accurate diagnosis is the cornerstone of effective treatment. The diagnostic process often involves a comprehensive evaluation, including a detailed psychiatric history, a physical examination to rule out underlying medical conditions, and sometimes, psychological testing. A thorough history of the patient's mood fluctuations, family history of mental illness, and any substance use is essential. Collateral information from family members or close friends can also provide valuable insights. The diagnostic process calls for open communication and honest self-assessment. The journey toward accurate diagnosis can be lengthy, but its value cannot be overstated.
Medication and Therapy: The Pillars of Effective Treatment
The treatment of bipolar depression typically involves a combination of medication and psychotherapy. Mood stabilizers, such as lithium and certain anticonvulsants, form a cornerstone of treatment, helping to regulate mood swings. Antidepressants can be added, but their use requires careful monitoring, as they can sometimes trigger or exacerbate manic episodes. Psychotherapy, including cognitive-behavioral therapy (CBT) and interpersonal and social rhythm therapy (IPSRT), plays a crucial role in helping patients manage their symptoms, develop coping mechanisms, and improve their overall quality of life. Individualized treatment plans are critical. Medication and therapy are not mutually exclusive; they are complementary tools that, when used together, can provide optimal outcomes.
Confronting the Stigma: Breaking Down Barriers
The stigma surrounding mental illness remains a significant obstacle to seeking and receiving help. Fear of judgment, shame, and discrimination can prevent individuals from reaching out for support. Education, advocacy, and open conversations are crucial to breaking down these barriers. By increasing awareness, challenging misconceptions, and promoting empathy, we can create a more supportive environment for those struggling with bipolar disorder. Let us work together to eliminate the stigma and foster a society where mental health is valued and prioritized.
The Urgent Need for Early Intervention
Early intervention is paramount. The longer bipolar disorder goes untreated, the more likely it is to cause profound disruption to a person's life. Early diagnosis and treatment can mitigate the severity of symptoms, reduce the risk of complications, and improve the chances of recovery. Recognizing the early warning signs, such as changes in mood, sleep patterns, and behavior, is crucial. Seeking help from a mental health professional at the first sign of trouble is a courageous and vital step. Early intervention can make a significant difference in the long-term outcome.
The Vital Role of Support Systems
The power of support systems in navigating the challenges of bipolar depression cannot be underestimated. Family, friends, support groups, and therapists can provide a vital source of strength, understanding, and encouragement. Building a strong support network is essential for long-term well-being. It is an investment in your future.
The Ever-Evolving Landscape of Treatment
Research continues to shed new light on the complexities of bipolar disorder, opening the door for advancements in treatment. Novel medications, innovative therapeutic approaches, and personalized interventions are constantly being developed. Staying informed about the latest developments can empower patients and their families to make informed decisions about their care. The future holds promise of more effective and individualized treatments, offering hope to those struggling with this challenging condition.
Looking Ahead: Hope and Healing
Bipolar depression is a formidable adversary, but it is not an insurmountable one. With accurate diagnosis, comprehensive treatment, unwavering support, and a commitment to self-care, individuals can live fulfilling lives. It's important to remember that recovery is not always linear; setbacks may occur. However, with persistence, resilience, and the unwavering belief in the possibility of healing, it is possible to reclaim your life. The journey may be challenging, but it is a journey worth taking. Embrace the hope.
