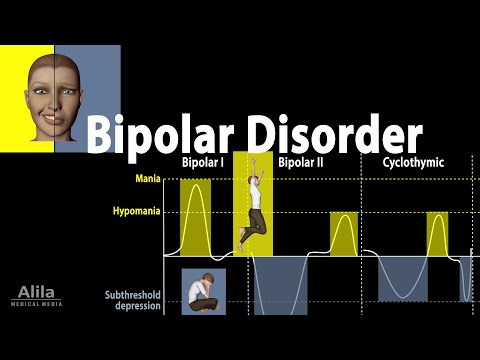
Title: Bipolar Disorder Symptoms, Risk Factors, Causes, Diagnosis and Treatments, Animation
Channel: Alila Medical Media
Bipolar Disorder Symptoms, Risk Factors, Causes, Diagnosis and Treatments, Animation by Alila Medical Media
major depressive disorder bipolar type 2, major depression vs bipolar 2, is bipolar 2 bipolar depression, can you have both bipolar disorder and major depressive disorder, difference between bipolar 2 and major depressive disorder
MDD & Bipolar II: The Shocking Truth Doctors Don't Want You to Know
Unmasking the Shadows: Decoding MDD and Bipolar II
This isn't your typical medical treatise. Prepare yourself for a journey. We'll explore the entwined realms of Major Depressive Disorder (MDD) and Bipolar II. It's about unveiling complexities that sometimes stay hidden. You're about to uncover insights. These insights might reshape your perspective.
The Elusive Dance: Understanding the Core Issues
MDD, often a relentless shadow, casts a dark blanket. It smothers joy and saps energy. It can feel like an inescapable prison. However, it's vital to note something crucial. Bipolar II, a more nuanced condition, complicates the picture. It’s characterized by both depression and hypomania. Hypomania is a state of elevated mood and energy. It is significantly different from full-blown mania. The distinctions are key. They are crucial for effective treatment.
Untangling the Web: Identifying the Overlapping Symptoms
The overlap between MDD and Bipolar II can be perplexing. Many symptoms are similar. Both can include persistent sadness. Both also have fatigue and hopelessness. However, there's a crucial difference. With Bipolar II, hypomanic episodes are present. These episodes involve increased activity. There's also a surge in energy and impulsivity. In contrast, MDD typically presents with a consistent state of depression. Diagnosis therefore hinges on careful observation. It requires detailed patient history. The goal here is to distinguish between the two.
Beyond the Surface: Unveiling the Diagnostic Challenges
Diagnosis often isn't straightforward. The diagnostic process can be lengthy. It demands patience and expertise. Furthermore, the subtle nuances of Bipolar II often get overlooked. It's sometimes misdiagnosed as MDD. Such misdiagnosis can hinder effective treatment. It is essential for doctors to consider this. They need to be meticulous. They must look for the cyclical nature of mood shifts. Accurate diagnosis shapes treatment plans. It drastically improves patient outcomes.
Navigating the Maze: The Impact on Daily Life
Living with either condition poses significant challenges. MDD profoundly impacts daily life. Tasks become overwhelming. Motivation fades. Social interactions become difficult. Similarly, Bipolar II affects routines. Hypomanic episodes can lead to risky behaviors. Depression then rears its head, leading to a cascade of emotional pain. These conditions significantly impact relationships. They affect work and even self-care. Therefore, coping mechanisms are absolutely necessary. Support systems are indispensable.
Weaving the Treatment Tapestry: A Holistic Approach
Treatment requires a multifaceted approach. It merges medication and therapy. Antidepressants are often used for MDD. However, in Bipolar II, they can trigger hypomania. Stabilization is the priority. Mood stabilizers are therefore crucial. Therapy provides vital support. Cognitive-behavioral therapy (CBT) can help. It teaches coping techniques. Interpersonal therapy (IPT) supports improved relationships. It offers valuable insights. This therapy approach helps manage the condition effectively.
Empowering Yourself: Strategies for Self-Care
Self-care is not an indulgence. It's a necessity. Consistent routines are essential. Prioritize sleep. Eat a balanced diet. Regular exercise is very beneficial. Mindfulness practices can help manage stress. Also, seek support from loved ones. Join support groups. Educate yourself about the condition. Taking charge of your health empowers you. These strategies significantly boost well-being.
The Road Ahead: Hope and Resilience
The journey can be challenging. But it's important to remember something. Hope remains. Recovery is possible. With proper treatment, management is achievable. Embrace support systems. Cultivate resilience. Every day, you’re one step closer to wellness. This road is about understanding and growth. It demands patience and self-compassion. Embrace the journey. You are not alone.
Escape the Darkness: Revolutionary Depression Nasal SprayMDD & Bipolar II: The Shocking Truth Doctors Don't Want You to Know
We live in a world obsessed with labels. We categorize everything – from the groceries we buy to the emotions we feel. When it comes to mental health, these categories, or diagnoses, become incredibly important. They guide treatment plans, influence the medications we take, and shape how we understand ourselves. Today, we're diving deep into two significant players in the mental health arena: Major Depressive Disorder (MDD) and Bipolar II Disorder. But here's the catch: there's a side to these conditions that often gets glossed over, a truth that sometimes even doctors struggle to fully acknowledge. This is what we’re unraveling today, the “shocking” truth.
1. The Great Misdiagnosis Game: Why It Matters
Let's be honest, diagnosing mental illness isn't like diagnosing the flu. There's no simple blood test or X-ray. We’re dealing with complex emotional and behavioral patterns. This is where the misdiagnosis game begins. Sometimes, the initial presentation of symptoms, especially in the early stages, can look remarkably similar across different conditions. MDD, for example, can often mimic the depressive phases of Bipolar II. This is like mistaking a flickering candle for a roaring bonfire – both produce light and heat, but one is a controlled burn while the other could engulf everything.
Why does misdiagnosis matter? Because the treatments for MDD and Bipolar II are very different. Antidepressants, the go-to medication for MDD, can actually trigger manic or hypomanic episodes in someone with undiagnosed Bipolar II, potentially making their condition significantly worse. Imagine trying to put out a fire with gasoline!
2. Unmasking MDD: Beyond the Gloom
Most of us are familiar with the classic hallmarks of MDD: persistent sadness, loss of interest in activities, fatigue, sleep disturbances, and changes in appetite. It often feels like a heavy, unwelcome blanket that smothers everything vibrant in your life. It can be a crippling experience, and we need to acknowledge it head-on.
3. Bipolar II: The Rollercoaster Nobody Asked For
Bipolar II, on the other hand, involves periods of major depression alternating with periods of hypomania. Hypomania is a milder form of mania – think of it as a rapid speed boost rather than a full-blown crash. It can manifest as increased energy, creativity, elevated mood, impulsivity, and a decreased need for sleep. The problem? These hypomanic episodes can feel incredibly good, but they can also lead to poor decision-making, reckless behavior, and strained relationships. Imagine riding a rollercoaster; the highs can be exhilarating, but the lows… they can be brutal.
4. The Overlap: When Lines Blur
Here's where things get tricky: the overlap. Both MDD and Bipolar II involve depression. This can make distinguishing between the two exceptionally difficult, especially when a person isn't actively experiencing hypomania. The subtleties of a medical interview and the patient's disclosures are very critical.
5. The Subtle Clues: Unveiling Hidden Patterns
So, how can you tell the difference? It's not always easy, but certain clues can point towards Bipolar II. Watch out for:
- Family History: A family history of Bipolar Disorder is a big red flag. Genetics play a significant role in both disorders.
- Antidepressant Response: Did antidepressants work initially? If they triggered hypomanic symptoms, that's often a strong indicator of Bipolar II.
- Cycles and Seasons: Do your mood swings seem to follow a cyclical pattern, possibly aligning with seasons or other triggers?
- Impulsivity: Are you prone to impulsive behaviors during periods of elevated mood?
- Racing Thoughts and Increased Energy: Do you have periods of rapid thinking or a sudden surge of energy and euphoria?
6. The Shocking Truth: Antidepressants Aren't Always the Answer
This is the truth that many doctors don't fully emphasize: antidepressants aren't a one-size-fits-all solution. While they are effective for many people with MDD, they can be detrimental for those with undiagnosed Bipolar II. They can worsen the condition by triggering or increasing the intensity and frequency of hypomanic episodes. It's like trying to force a square peg into a round hole; it just doesn't work, and it will likely damage the peg in the process.
7. The Stigma Factor: Why People Hide Symptoms
Let’s not forget the elephant in the room: stigma. Mental health struggles, unfortunately, still carry a heavy burden of shame. This can make people hesitant to seek help or to honestly share their experiences with doctors. Imagine trying to explain the complex workings of your heart to a doctor in a room of strangers when you're feeling very vulnerable and ashamed. This only can lead to a delay in diagnosis and treatment.
8. The Importance of a Thorough Assessment
This brings us to the critical importance of a comprehensive diagnostic assessment. This isn’t just a quick chat; it involves a detailed review of your symptoms, medical history, family history, and possibly psychological testing. It's about taking a deep dive, like a seasoned detective piecing together clues to solve a complex mystery.
9. Beyond Medication: Holistic Approaches
While medication can be a critical component of treatment for both MDD and Bipolar II, it's not the only answer. Therapy, particularly cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT), can give you tools to manage your emotions, behaviors, and relationships, like having a toolbox to work on your own car! Lifestyle adjustments, such as regular exercise, a healthy diet, and sufficient sleep, can also make a big difference.
10. Finding the Right Support: A Team Effort
Navigating mental health challenges is rarely a solo journey. Find the support you need - whether it’s from a trusted therapist, a supportive friend or family member, or a peer support group. Build a solid support system to assist you in your journey.
11. Open Communication: The Key to Success
Honest and open communication with your mental health professional is paramount. Be transparent about your symptoms, your experiences, and your reactions to medications. Don’t be afraid to ask questions or seek a second opinion if you feel something isn't right.
12. The Patient's Role: Become Your Advocate
You are the expert on your own experience. Be an active participant in your care. Research resources, understand your rights, and advocate for yourself.
13. Challenging the Status Quo: Questioning Conventional Wisdom
Don't be afraid to challenge conventional thinking. Do your own research, and consider alternative perspectives. Mental health is not a simple science, and there is no single "right" way to treat everyone.
14. The Future of Mental Health Care
The future of mental health care lies in increased awareness, reduced stigma, and personalized treatment approaches. More research is needed, and we need to create a system that is more responsive to the specific needs of each individual.
15. Embracing the Journey: Hope and Resilience
Dealing with MDD or Bipolar II can feel like a marathon, not a sprint. It's about finding the right support, building resilience, and never giving up hope. This is a difficult path, but it can also lead to great personal growth and a deeper understanding of yourself.
In conclusion, we've peeled back layers of the complexities surrounding MDD and Bipolar II. We've highlighted the challenges of misdiagnosis, the importance of a thorough assessment, the risks of relying solely on antidepressants, and the power of holistic approaches. We've also discussed the very critical role open communication, patient advocacy, and a strong support system. Remember, you're not alone, and the journey towards healing and well-being is always worth undertaking.
FAQs
1. Can MDD turn into Bipolar II?
No, MDD cannot turn into Bipolar II. However, it's possible that someone initially diagnosed with MDD may actually have undiagnosed Bipolar II. This becomes apparent when they react poorly to antidepressants or when hypomanic symptoms surface.
2. What if I suspect I have Bipolar II, but my doctor only diagnosed me with MDD?
Speak candidly with your doctor about your concerns. Describe your symptoms in detail, especially any history of periods of increased energy, impulsivity, or decreased need for sleep. If you aren't satisfied, seek a second opinion from a psychiatrist or a mental health professional specializing in mood disorders.
3. What are the common medications used to treat Bipolar II?
Mood stabilizers (such as lithium, lamotrigine, and valproic acid) are frequently used to treat Bipolar II. Antidepressants may be used cautiously, often in combination with a mood stabilizer, but their use must be carefully monitored.
4. How long will I need to take medication for Bipolar II?
Bipolar II is a chronic condition. Most people with Bipolar II require ongoing medication to manage their symptoms and prevent relapses. The duration of treatment varies depending on the individual and their response to medication.
5. Is therapy necessary for Bipolar II?
Yes, therapy is frequently a key component of a comprehensive treatment plan for Bipolar II. Therapy, like CBT or DBT, can help you manage your emotions, develop coping skills, identify triggers, and improve your relationships.
**Principal
Is Your Depression CAUSING This SHOCKING Joint Pain?Bipolar 2 looks like depression anxiety, making it hard to diagnose

By Kojo Sarfo, DNP Bipolar 2 looks like depression anxiety, making it hard to diagnose by Kojo Sarfo, DNP
Depressive and Bipolar Disorders Crash Course Psychology 30

By CrashCourse Depressive and Bipolar Disorders Crash Course Psychology 30 by CrashCourse

Title: Bipolar 1 Disorder or Bipolar 2 Disorder - Which is Worse
Channel: Dr. Tracey Marks
Bipolar 1 Disorder or Bipolar 2 Disorder - Which is Worse by Dr. Tracey Marks
Japan's Hidden Depression: The Shocking Truth Behind the 😔 Emoji
MDD & Bipolar II: Unmasking the Complexities Doctors Often Overlook
We understand the daunting journey of navigating mental health diagnoses. The terrain is often complex, riddled with misinformation and, at times, a frustrating lack of clarity. When facing a suspected diagnosis of Major Depressive Disorder (MDD) or Bipolar II, the path can feel even more treacherous. It’s a landscape etched with fluctuating moods, challenging treatments, and the persistent quest for the right answers. This exploration, crafted with meticulous attention to detail, is intended to illuminate the often-overlooked subtleties within these conditions, providing a deeper understanding than what’s commonly presented.
The Elusive Nature of Misdiagnosis: Why MDD and Bipolar II Can Overlap
The core challenge in differentiating between MDD and Bipolar II—and the reason misdiagnosis is alarmingly common—lies in their shared features and the nuanced presentation of symptoms. Both conditions prominently display depressive episodes. However, the key delineator of Bipolar II is the experience of hypomanic episodes, distinct periods of elevated mood, increased energy, and altered thinking that are less severe than full-blown mania. These hypomanic episodes, often subtle and fleeting, can easily slip beneath the radar, leading clinicians to overlook the bipolar spectrum altogether.
Consider a patient presenting with persistent feelings of sadness, loss of interest, sleep disturbances, and fatigue—classic MDD symptoms. If a clinician focuses solely on these depressive aspects, a diagnosis of MDD might seem logical. However, if the patient also experiences periods of increased productivity, heightened creativity, rapid speech, or impulsive behavior, even for a few days, this strongly suggests the presence of hypomania and, consequently, Bipolar II. The problem is the diagnostic process is often fragmented, lacking the detailed, longitudinal assessment required to catch these subtle telltale signs.
The frequency, duration, and intensity of these hypomanic episodes are critical. Hypomania, by definition, does not involve psychosis or require hospitalization. It’s often experienced as a positive force, a surge of energy and drive. This can lead individuals to discount or downplay the significance of these episodes, further obscuring the true nature of their condition. Family observations, detailed mood charting, and thorough patient history are pivotal in uncovering the truth.
The Impact of Untreated or Mismanaged Bipolar II
The consequences of misdiagnosing and subsequently inadequately treating Bipolar II can be profoundly damaging. While MDD treatments, such as antidepressants, can be life-saving for those with unipolar depression, they can be problematic—even counterproductive—for those with an underlying bipolar disorder. Antidepressants, when used alone in Bipolar II, can trigger hypomania, potentially escalating into full-blown mania, or can lead to rapid cycling, where mood swings become significantly more frequent and intense.
Beyond these therapeutic concerns, the psychosocial ramifications of untreated Bipolar II are significant. The unpredictable nature of mood episodes can strain relationships, disrupt work or academic performance, and escalate the risk of substance abuse as individuals self-medicate in an attempt to manage their symptoms. Furthermore, there's an elevated risk of suicidal ideation and attempts in individuals with Bipolar II, emphasizing the urgency of accurate diagnosis and effective treatment.
The economic costs are also substantial. Lost productivity, healthcare utilization, and the need for more intensive levels of care contribute to the burden on individuals, families, and society. This includes, too, hospitalization, which is frequently associated with the misdiagnosis.
Unveiling the Hypomanic Spectrum: Beyond the Surface Symptoms
Hypomania isn't a singular phenomenon. It exists on a spectrum, and its presentation can vary significantly from one individual to another. While some individuals experience the classic hallmarks of increased energy, impulsivity, and elevated mood, others may exhibit less obvious symptoms, such as subtle shifts in thinking, heightened creativity, or a greater need for social interaction.
Consider someone who usually values routine but suddenly embraces spontaneous travel plans and makes impulsive purchases. Or someone who is characteristically quiet now regularly dominates conversations. These subtle behavioral changes, often attributed to personality quirks or temporary stress, can be red flags of underlying hypomania.
Specific examples can help clarify the varied presentations, and we must be very detailed:
- Cognitive Shifts: These include racing thoughts, distractibility, and a subjective feeling of heightened mental acuity. An individual may experience an increase in creativity, generating ideas at a rapid pace. This can manifest in artistic pursuits, work projects, or simply in rapid-fire conversations.
- Behavioral Changes: Increased activity levels, such as pacing, restlessness, or an inability to sit still, may be present. There can be an increased interest in pleasurable activities, such as excessive shopping, gambling, or engaging in risky behaviors. Additionally, there might be a decreased need for sleep, often needing just a few hours a night while still functioning effectively.
- Mood Variability: While hypomania is characterized by an elevated or expansive mood, it can also present with irritability or an unusually short temper. Individuals may become more talkative, outgoing, and sociable, but this can easily morph into argumentativeness.
The Crucial Role of Comprehensive Assessment and Accurate Diagnosis
Obtaining an accurate diagnosis of MDD or Bipolar II demands a comprehensive evaluation, moving beyond a simple checklist of symptoms. This process should involve multiple steps:
Thorough Psychiatric Evaluation: A detailed discussion with a psychiatrist or qualified mental health professional is essential. This should include a review of past medical history, family history of mental illness, and a detailed exploration of current symptoms, including the nature, duration, frequency, and severity of mood episodes.
Mood Charting and Symptom Tracking: Patients should maintain a mood diary to track their mood fluctuations, sleep patterns, energy levels, and any other relevant symptoms. This provides invaluable data for identifying patterns and potential hypomanic episodes that may have been missed during a single clinical interview.
Collateral Information: Gathering input from family members, friends, or close colleagues can provide valuable insights into the individual’s behavior and any subtle changes that the individual themselves may be less aware of.
Differential Diagnosis Considerations: The clinician must differentiate Bipolar II from other mental health conditions that can present with similar symptoms, such as borderline personality disorder, attention-deficit/hyperactivity disorder (ADHD), and substance use disorders.
Ongoing Monitoring: Mental health is dynamic, and assessments must not be a one-time event. Regular follow-up appointments are vital to monitor treatment effectiveness, assess for any changes in symptoms, and adjust treatment plans as needed.
Treatment Strategies: Tailoring Care for Optimal Results
Effective treatment for Bipolar II typically combines medication and psychotherapy.
Medication: Mood stabilizers, such as lithium or certain anticonvulsants (e.g., lamotrigine), are the cornerstone of treatment for Bipolar II. These medications help regulate mood swings and reduce the frequency and severity of both depressive and hypomanic episodes. Antidepressants should be used with caution and preferably in conjunction with a mood stabilizer to mitigate the risk of triggering hypomania or rapid cycling.
Psychotherapy: Various forms of psychotherapy, such as cognitive-behavioral therapy (CBT) and interpersonal and social rhythm therapy (IPSRT), can be highly effective in managing Bipolar II. CBT helps individuals identify and change negative thought patterns and behaviors. IPSRT focuses on establishing regular daily routines to stabilize mood. Family therapy can also be beneficial, providing support and education for both the individual and their loved ones.
Lifestyle Modifications: Integrating healthy lifestyle habits, such as regular exercise, a balanced diet, adequate sleep, and stress-management techniques, can play a crucial role in stabilizing mood and enhancing treatment outcomes. It is particularly important to limit or avoid alcohol and illicit drugs, as these can exacerbate mood swings.
Collaborative Approach: Treatment is most effective when the individual, their therapist, and their psychiatrist work collaboratively. Open communication and shared decision-making are critical in developing a treatment plan that meets the individual's specific needs. Careful review and open conversation of side effects.
Empowerment Through Knowledge: A Path Forward
Understanding the intricacies of MDD and Bipolar II, recognizing the potential for misdiagnosis, and actively seeking the right kind of care are vital steps in navigating these conditions. This is where an informed approach, combined with the support of qualified healthcare professionals, makes all the difference.
By embracing knowledge, meticulously tracking symptoms, and proactively engaging in treatment, individuals with MDD and Bipolar II can significantly improve their quality of life, manage their symptoms, and embark on a path toward lasting well-being. Never underestimate the power of self-advocacy—asking questions, demanding thorough evaluations, and finding clinicians who truly listen and understand your unique experience. With the right information and support, the journey through these sometimes-complex conditions becomes not just manageable but can lead to a fulfilling life.

